|
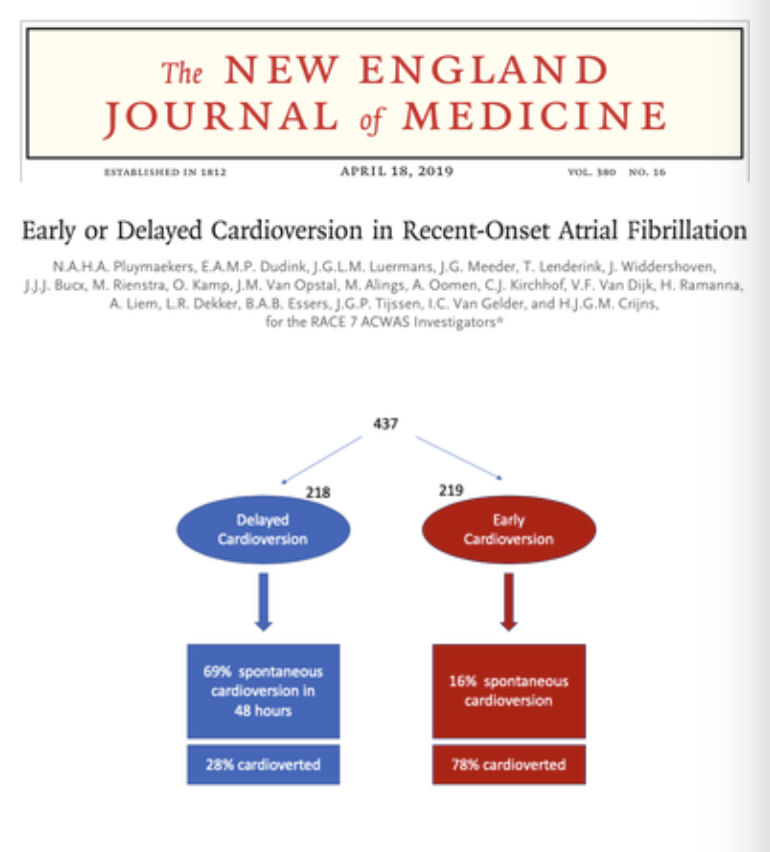
Atrial Fibrillation(AF) is the most common Emergency Department Arrhythmia you will see. Patients have a lifetime risk approaching 25% of having this. However as prevalent as this arrhythmia is and as many studies as have been done, looking at its management, it is still an area (certainly in the area of recent onset AF). Perhaps the title of the paper on the right, best illustrates the confusion I'm talking about.
|
OBJECTIVES OF THIS MODULE
In this module we want to look at 2 patient types:
Answer the questions and then watch the 5 minute summary video at the end to bring it all together.
In this module we want to look at 2 patient types:
- The stable patient with AF of less than 48 hours duration
- The unstable AF patient
Answer the questions and then watch the 5 minute summary video at the end to bring it all together.
RISK FACTORS FOR ATRIAL FIBRILLATION
|
|
The Stable Patient with < 48 hours of AF
Answer the following questions first then move on down the page and look at the answers.
1. ALL PATIENTS WHO PRESENT TO THE ED WITH <48 HOURS OF AF SHOULD BE CARDIOVERTED. TRUE/FALSE?
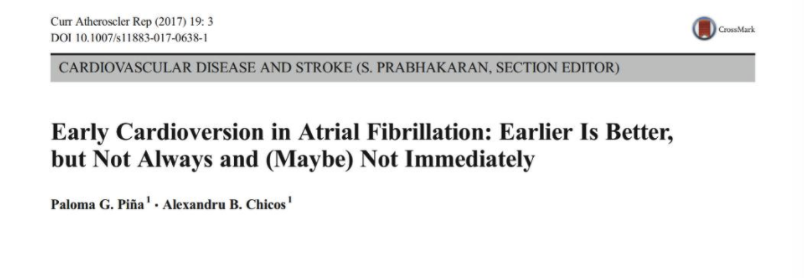
This is such a controversial topic. On the whole I would say it is FALSE. However read on for a review and you can surmise for yourself. A significant number of these patients will revert by themselves. Read On.
2. IF WE ARE AIMING FOR PHARMACOLOGICAL RHYTHM CONTROL IN THE ED, AMIODARONE IS THE DRUG OF CHOICE. TRUE/FALSE?
FALSE. Procainamide has a higher rate of rhythm control. Sometimes,certainly in Australia, it has been a difficult drug to find.
3. MAGNESIUM IS SUPERIOR TO AMIODARONE AND PROCAINAMIDE FOR RHYTHM CONTROL. TRUE/FALSE?
Magnesium Sulfate is a popular drug in the ED. It can slow the rate and if given too fast, can drop the blood pressure. In terms of rhythm control, it is no better than placebo.
The approach to the patient with < 48 hours of AF, depends on many things:
DC CARDIOVERSION(DCCV) vs PHARMACOLOGICAL CARDIOVERSION
It has a success rate of 89-97%. Those patients having DCCV have higher rates of discharge and shorter ED length of stays. It is also a relatively safe procedure. The sedation aspect, is something we do well in the ED.
Some of the potential complications include:
The complications are similar to DCCV.
Procainamide is said to have a 58% rate of cardioversion, compared to Amiodarone with a 50% rate of cardioversion.
- It can depend on the level of symptomatology, the patient is experiencing. Some patients have relatively few symptoms. Others might have symptoms they hate, which include, palpitations, a throbbing in the head etc and want rapid control
- Can the patient come back to the ED? A wait and see approach is an important alternative.
- Are they prepared to have cardioversion?
- Can they tolerate the medications?
DC CARDIOVERSION(DCCV) vs PHARMACOLOGICAL CARDIOVERSION
It has a success rate of 89-97%. Those patients having DCCV have higher rates of discharge and shorter ED length of stays. It is also a relatively safe procedure. The sedation aspect, is something we do well in the ED.
Some of the potential complications include:
- Respiratory Depression(up to about 4%)
- Bradycardia( 0.2%)
- Hypotension (1%)
- VT (1%)
- Thromboembolism (0.8%)
The complications are similar to DCCV.
Procainamide is said to have a 58% rate of cardioversion, compared to Amiodarone with a 50% rate of cardioversion.
THERE IS A NEED FOR DCCV OR PHARMACOLOGICAL CARDIOVERSION AS THE RATE OF SPONTANEOUS REVERSION IS LOW. TRUE/FALSE?
FALSE. The rate of spontaneous cardioversion is significant. Read on, below for a summary.
Let's look at the approach to a patient with AF<48hours in terms of DCCV.
CASE. BEFORE WE BEGIN THIS SECTION THINK ABOUT THE FOLLOWING CASE........
A 48 you male with no past medical history presents to the emergency department at 10pm with onset of palpitations. He has a throbbing feeling in his head, however apart from this is comfortable, with no shortness of breath and no chest discomfort.
He gives a history of the palpitations starting sharply about 1.5 hours ago. He still feels them. He has no past history of palpitations.
His vitals are:
Here are some questions to consider:
He gives a history of the palpitations starting sharply about 1.5 hours ago. He still feels them. He has no past history of palpitations.
His vitals are:
- HR 158 bpm
- BP 134/68
- Sats on room air 99%
Here are some questions to consider:
- Will you try and Cardioversion this patient immediately?
- Is there a place for sending him home and seeing if he spontaneously cardioverts.
- If you decide on either approach, what is his rate of stroke and will you anticoagulate in each instance?
|
If we look at the literature, we know that 50-60% of patients revert on their own, if we do nothing. We also know that about 15% will return to AF after reversion.
If the patient can tolerate the symptoms and are happy to go home and return the next day for review and be cardioverted then, if they haven't self reverted, this may have some benefits. Let's put aside the issues of inconvenience to the patient, extra work the next day in the ED and the relative safety of DCCV. If we cardiovert all-comers then we are cardioverting about twice as many patients as we need to, given that about half the patients will revert by themselves. |
Is there a stroke risk if we delay cardioversion?
Thromboembolic Complications After Cardioversion of Acute Atrial Fibrillation. The FinCV Study JACC, Volume 62, Issue 13, September 2013
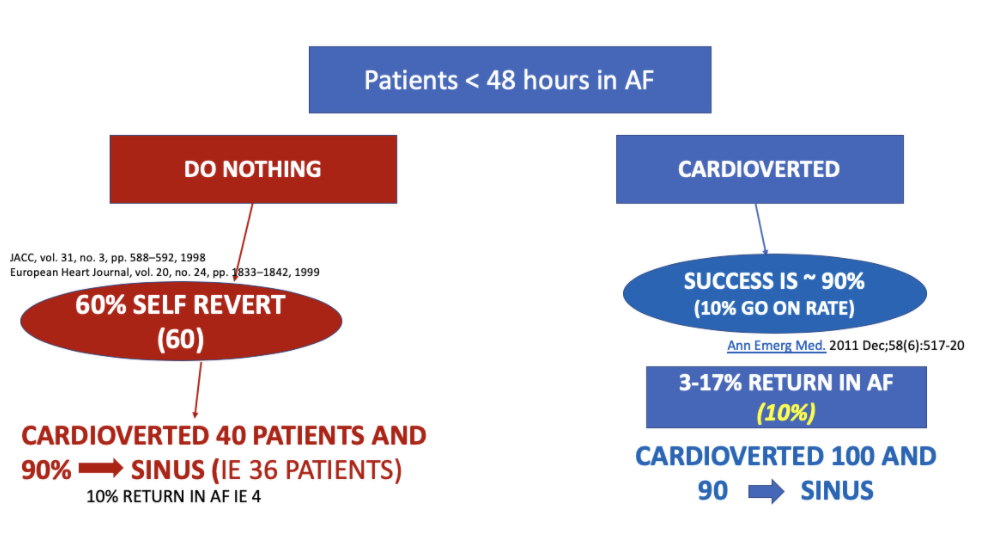
In the above study it was found that Stroke risk and time to cardioversion were related in the following way: < 12 hours: 0.3% 12-48 hours: 1.1% Several risk factors were also found to help in predicting stroke risk.
if AGE >60 + heart failure + Diabetes: risk is 9.8% In patients with AF for < 48 hours, the risk of stroke is 0.7-1.1%, mainly in patients with risk factors- what are they? |
If score > 2- anticoagulate as >2.2% chance of stroke
Warfarin in mitral stenosis and mechanical heart valves DOAC decreases stroke rate and decrease rate of bleeding APIXABAN: less bleeding risk
|
|
In this NEJM article in 2019 they randomised 437 patients to:
Their findings were quite interesting:
In those where cardioversion was delayed:
|
This trial found that delayed cardioversion was not inferior to early cardioversion.
An approach would be to use this, in a shared decision model with the patient. However to minimise risk, by using it only for those that did not qualify as high risk ie., age, heart failure diabetes etc....Should we anticoagulate patients we are going to cardiovert?“we suggest starting anticoagulation at presentation (low-molecular-weight heparin or unfractionated heparin at full venous thromboembolism treatment doses) and proceeding to cardioversion ……..
After successful cardioversion to sinus rhythm, we recommend therapeutic anticoagulation for at least 4 weeks rather than no anticoagulation, regardless of baseline stroke risk (Grade 2C). “
Chest Journal February 2012, Vol 141, No. 2_suppl
There is no real consensus in the guidelines. Some recommend peri-cardioversion for all. Some risk stratify(as above based on age and risk factors). In ACC 2014 they risk stratify patients into: low and high risk of thromboembolism. Those at low risk don't need anticoagulation. Those at high risk need pericardioversion anticoagulation and anticoagulation for 4 weeks post cardioversion.
Follow your hospitals protocols, in unison with your cardiology unit.
After successful cardioversion to sinus rhythm, we recommend therapeutic anticoagulation for at least 4 weeks rather than no anticoagulation, regardless of baseline stroke risk (Grade 2C). “
Chest Journal February 2012, Vol 141, No. 2_suppl
There is no real consensus in the guidelines. Some recommend peri-cardioversion for all. Some risk stratify(as above based on age and risk factors). In ACC 2014 they risk stratify patients into: low and high risk of thromboembolism. Those at low risk don't need anticoagulation. Those at high risk need pericardioversion anticoagulation and anticoagulation for 4 weeks post cardioversion.
Follow your hospitals protocols, in unison with your cardiology unit.
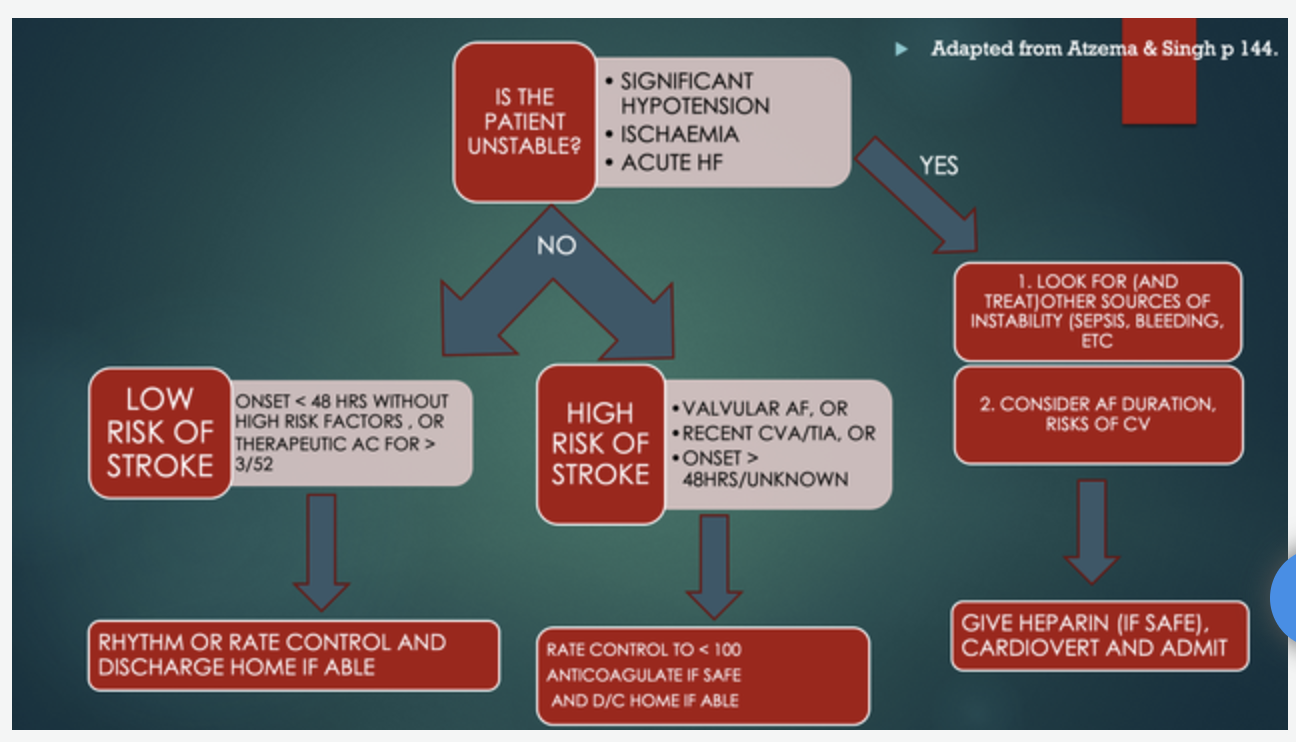
What about the UNSTABLE AF patient?
Unstable is defined as that patient that is:
These patient usually have a heart rate > 150.
Most guidelines will recommend DCCV.
What we need to remember is that the AF is rarely the cause of the hypotension(perhaps if very high rates), however we need to look at the causes of SHOCK. We need to treat these causes ie., sepsis, pulmonary embolism, hypoxia, hypovolaemia.
If no other cause is apparent, then consider the use of DCCV.
Beware in the patient with a known poor ejection fraction as atrial stunning post cardioversion can continue to drop the BP.
An Approach to the AF Patient
Atzema C,L, Singh SM. Acute Management of Atrial Fibrillation:From Emergency Department to Cardiac Care Unit. Cardiol Clin. 2018 Feb;36(1):141-159. doi: 10.1016/j.ccl.2017.08.008.Epub 2017 Oct 23.
Unstable is defined as that patient that is:
- hypotensive
- has ischaemic chest pain
- has developed heart failure
These patient usually have a heart rate > 150.
Most guidelines will recommend DCCV.
What we need to remember is that the AF is rarely the cause of the hypotension(perhaps if very high rates), however we need to look at the causes of SHOCK. We need to treat these causes ie., sepsis, pulmonary embolism, hypoxia, hypovolaemia.
If no other cause is apparent, then consider the use of DCCV.
Beware in the patient with a known poor ejection fraction as atrial stunning post cardioversion can continue to drop the BP.
An Approach to the AF Patient
Atzema C,L, Singh SM. Acute Management of Atrial Fibrillation:From Emergency Department to Cardiac Care Unit. Cardiol Clin. 2018 Feb;36(1):141-159. doi: 10.1016/j.ccl.2017.08.008.Epub 2017 Oct 23.
Watch this rapid summary of the topic by Dr Adam Michael.