CASE
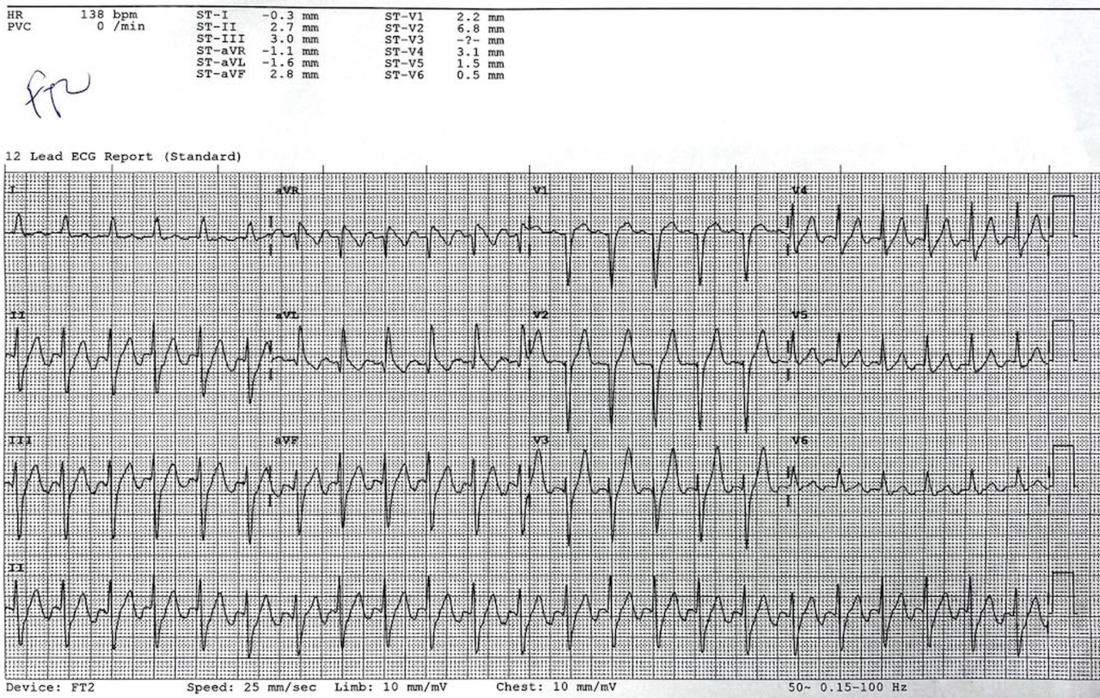
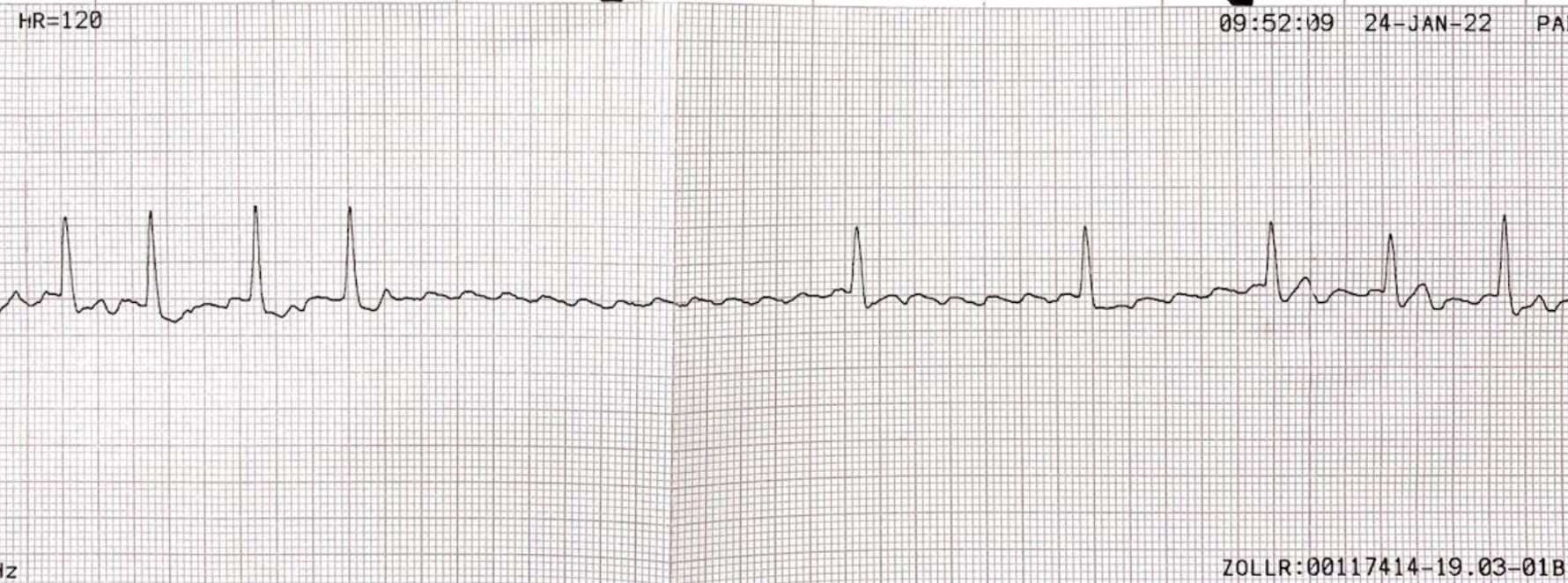
A 78 yo patient male presents with palpitations. He has no chest pain or shortness of breath. His heart rate is 138bpm and he was haemodynamically stable.
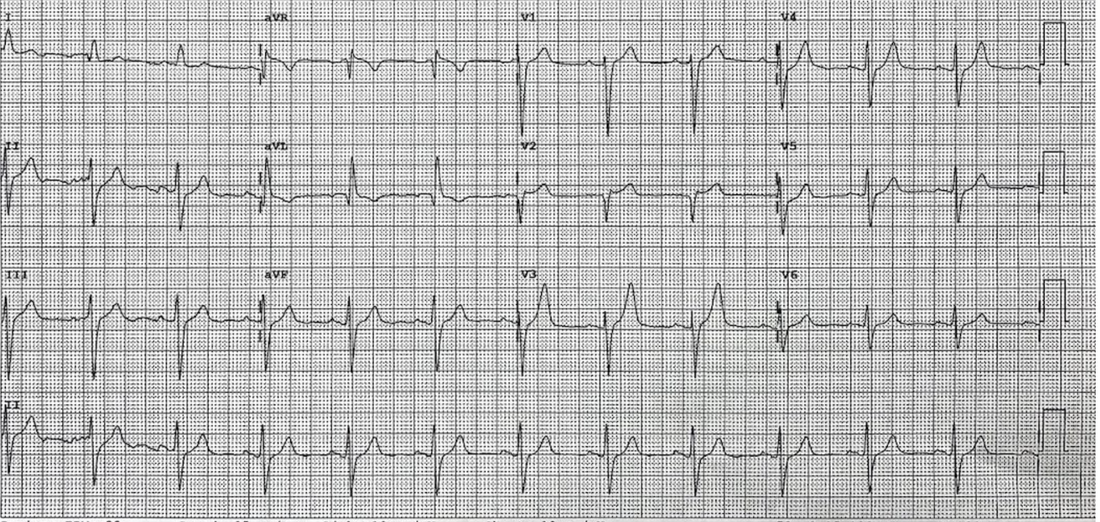
His ECG is shown below. Discuss and interpret the ECG.
His ECG is shown below. Discuss and interpret the ECG.
What does the ECG show?
|
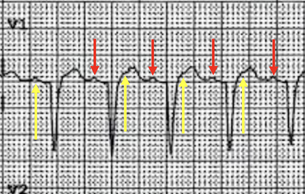
If we look at the rate it is 138bpm. In lead one there is a p wave clearly seen. We can easily mistake this for sinus rhythm, if we were only looking at the ECG. Remember that the ECG is a snapshot in time. If we look at the monitor, it is exquisitely regular ie., it does not change at all. This cannot really be atrial flutter. Could there be a p wave hidden in the T wave?
|
Sometimes turning the ECG upside down can help us to see the flutter waves. Although this is not always obvious.
Our Management
|
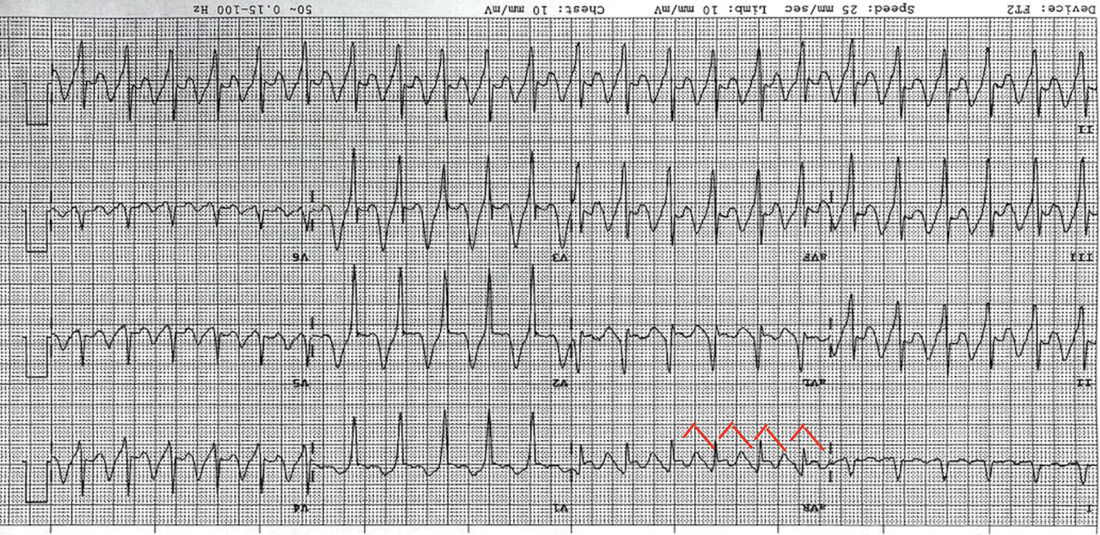
The patient was stable. Because we were not sure of the rhythm and were thinking of an SVT, we gave the patient Adenosine. This unmasked the atrial flutter.
We attempted vagal manoeuvres, but know that they almost never work. We decided to DC cardiovert the patient. It was a uneventful procedure and the patient returned to normal sinus rhythm. |
ATRIAL FLUTTER
Second most common arrhythmia we will see, after atrial fibrillation
It is macroreentrant atrial tachycardia with the loop above the AV node in the right atrium. Complexes are narrow.
The AVN cannot conduct at the same rate (240-360) as the flutter, so have a block:
It is macroreentrant atrial tachycardia with the loop above the AV node in the right atrium. Complexes are narrow.
- type 1 flutter is the most frequent. In this type of flutter, right atrial activation rotates in a counterclockwise direction.
The AVN cannot conduct at the same rate (240-360) as the flutter, so have a block:
- 1:1, which can be unstable
- 2:1, which is the most common
- 3:1
- 4:1
- It can also be variable which gives the appearance of an irregular rhythm.
How do we distinguish between Atrial flutter and:
- Sinus Tachycardia: This may be tricky, as we will sometimes only see one P wave. (see case below). The biggest difference will be that when we look at the monitor, the rate will change in sinus tachycardia, however in atrial flutter the rate will be regular.
- Atrial Tachycardia: Rates are usually > 100bpm
CAUSES
Think of any causes that dilate the atrium:
Think of any causes that dilate the atrium:
- Left sided CCF
- PE
- Left sided valvular heart disease especially tricuspid and mitral valves
- Septal defects
- Hyperthyroidism
- Increased alcohol intake
MANAGEMENT
ED Management depends on the stability of the patient
UNSTABLE PATIENT
|
CARDIOVERSION
|
PHARMACOLOGICAL THERAPY
|
STABLE PATIENT
|
Can still use synchronised cardioversion
|
Can slow the ventricular response.
|
ANTITHROMBOTIC THERAPY
Antithrombotic therapy can be used in those patients with the same risk profile as atrial fibrillation
CHA2DS2-VASc
If CHADSVASc score is:
> 2 -Anticoagulate
1 - Aspirin or oral anticoagulants
0 - No antithrombotic therapy.
- Mechanical heart valves- Warfarin
- Non-valvular AF and history of previous stroke/TIA-warfarin or DOACs are recommended.
CHA2DS2-VASc
- CCF
- Hypertension
- Age>75
- DM
- Stroke/TIA/thromboembolismVascular disease
- Prior MI, PVD, aortic plaque
- Age 65-75
- Sex(female)
If CHADSVASc score is:
> 2 -Anticoagulate
1 - Aspirin or oral anticoagulants
0 - No antithrombotic therapy.