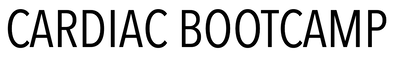
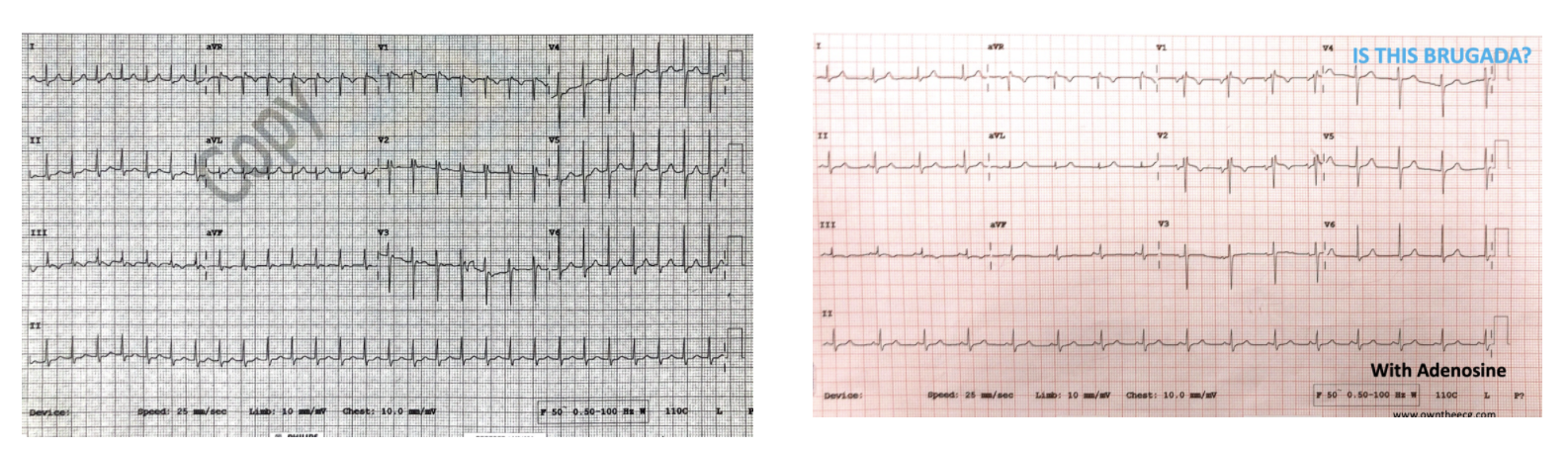
An 80 yo man presents with shortness of breath.
He is diagnosed with pneumonia.
This is his ECG.
Is this Brugada?
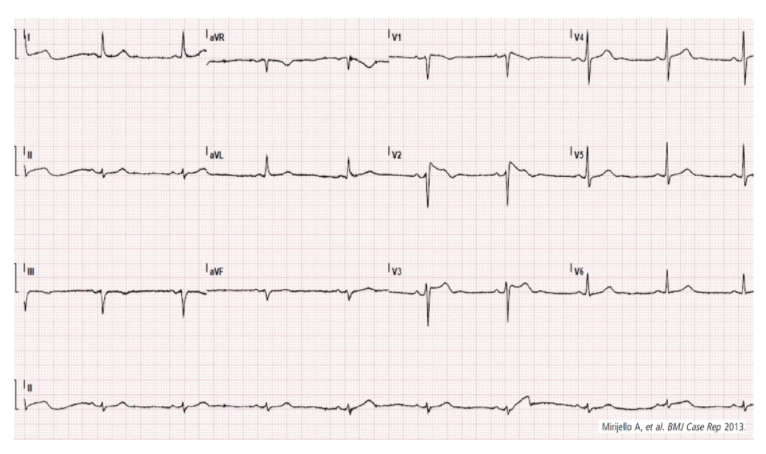
He is diagnosed with pneumonia.
This is his ECG.
Is this Brugada?
|
ECG WITH FEVER
|
ECG ON FEVER RESOLUTION
|
Case 2.
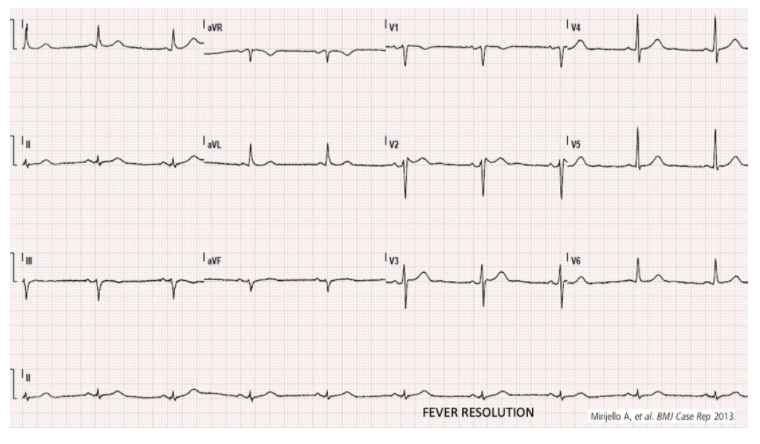
A 19 yo male presents with tachycardia. His ECG shows an SVT.
He is reverted with Adenosine.
His second ECG is suspicious of Brugada Syndrome. The registrar thinks it is.
How can we work out if it is Brugada?
What do you think? Is it?
He is reverted with Adenosine.
His second ECG is suspicious of Brugada Syndrome. The registrar thinks it is.
How can we work out if it is Brugada?
What do you think? Is it?
ANSWER
This is not Brugada. The patient was discharged home.
Read on to see how we diagnose Brugada.
Read on to see how we diagnose Brugada.
What is Brugada Syndrome?
It is an inherited autosomal dominant Na+ channel abnormality(1). It is far more common in males (by factor of 8-10:1) where it is the second most common cause of death in those less than 40 years of age. The true prevalence is difficult to estimate, as it is a dynamic ECG pattern, ie., it is not always present. It is usually associated with sudden death in those with structurally normal hearts.
It’s prevalence is about 5/10000 of the population, being responsible for approximately 4% of all sudden cardiac deaths. It has a high prevalence in South-East Asia and is the same disorder as the previously known Sudden Unexplained Nocturnal Death Syndrome(SUNDS)(2)
Patients may suffer sudden cardiac death, or present in cardiac arrest, usually with polymorphic ventricular tachycardia or ventricular fibrillation(VF) being the most common arrhythmias. Patients with the syndrome, may also present following a syncopal episode, which may be a result of self-termination of the arrhythmia.
Beware the patient whose partner or family member describe nocturnal agonal respirations, as VF and sudden death in Brugada usually occurs at night or at rest(2). This may be due to sympathovagal balance or bradycardia which may initiate the arrhythmia.
The high prevalence in Asian populations has seen specific language emerge to describe it’s occurrence at night(3):
The pattern is more likely to be seen in the following circumstances:
These changes seen in leads V1 or V2 or both are shown below.
It’s prevalence is about 5/10000 of the population, being responsible for approximately 4% of all sudden cardiac deaths. It has a high prevalence in South-East Asia and is the same disorder as the previously known Sudden Unexplained Nocturnal Death Syndrome(SUNDS)(2)
Patients may suffer sudden cardiac death, or present in cardiac arrest, usually with polymorphic ventricular tachycardia or ventricular fibrillation(VF) being the most common arrhythmias. Patients with the syndrome, may also present following a syncopal episode, which may be a result of self-termination of the arrhythmia.
Beware the patient whose partner or family member describe nocturnal agonal respirations, as VF and sudden death in Brugada usually occurs at night or at rest(2). This may be due to sympathovagal balance or bradycardia which may initiate the arrhythmia.
The high prevalence in Asian populations has seen specific language emerge to describe it’s occurrence at night(3):
- In Thailand, ‘Lai Tai’ was the term used to describe nocturnal deaths. The word “Lai” means a loud groan occurring in sleep and “Tai” means death.
- In the Philippines Bangungut, means “to rise and moan in sleep,” and describes the disease.
- In Japan, Pokkuri Death Syndrome, was similar, with “Pokkuri” meaning sudden, unexpected death.
- The diagnostic Brugada ECG pattern is present and
- There is a relevant clinical history.
The pattern is more likely to be seen in the following circumstances:
- Fever
- Intoxication
- Vagal Stimulation
- Electrolyte abnormality ; hyper/hypo K+, hyperCa2+
- Unmasked by Na+ channel blockers
- Medication related:
- Alpha agonists
- Beta blockers
- Tricyclic/tetracyclic antidepressants
- Antianginals
- Drug related: Cocaine toxicity
- Ischaemia
- Cardioversion: The ECG feature Type I pattern, can appear for a short period after cardioversion, although the significance of this is uncertain(4)
These changes seen in leads V1 or V2 or both are shown below.
|
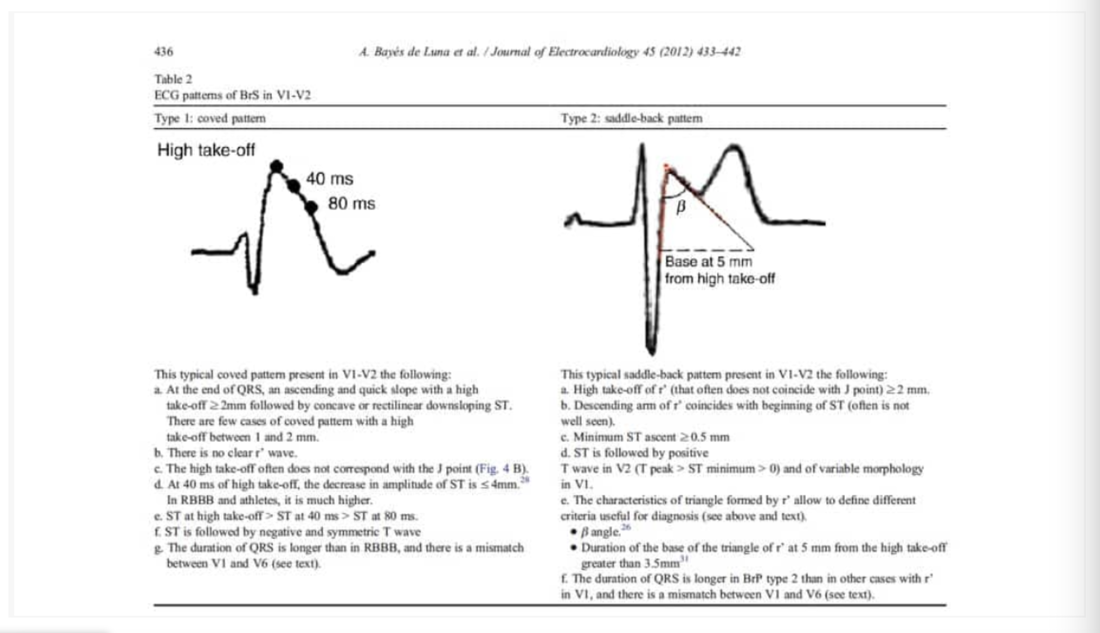
TYPE I: Coved PatternThis is a very specific pattern and in patients with no heart disease is highly specific for Brugada. The important elements of the pattern are:
|
TYPE II: Saddle-back patternThis pattern combines the previous Type II and III patterns into a new Type II pattern.
There must be an RSr’ pattern with a saddle-back morphology. The r’ is usually more than 2mm above the isoelectric line. The QRS duration in Brugada is greater in V1 than V6. This helps distinguish it from a RBBB where the QRS duration is similar in both these leads. This morphology can be a normal finding on ECGs. To distinguish a normal morphology from a saddle-back pattern of Brugada we need to calculate the beta angle as shown below. A wide beta angle (> 35 degrees) indicates a Brugada pattern. |
If there is a suggestion of a Brugada pattern in V1-V2, a further ecg should be performed with high precordial leads as shown. This simply means moving the leads V1 and V2 from the 4th intercostal spaces to the second or third. This allows the leads to be closer to the affected zone, which usually coincides with the RVOT and unmask the abnormality. We are looking for the Type I coved pattern to be unmasked in these high precordial leads.
Beware, that a false Type II Saddleback pattern can occur, if the V1 and V2 leads are placed too high. A clue to their misplacement is given by the P wave in V2. This should normally be upright. If it is not, then be suspicious of high leads and redo the ECG.
Beware, that a false Type II Saddleback pattern can occur, if the V1 and V2 leads are placed too high. A clue to their misplacement is given by the P wave in V2. This should normally be upright. If it is not, then be suspicious of high leads and redo the ECG.
Clinical Criteria
To make the diagnosis of Brugada Syndrome we need both the ECG patterns described above and the clinical features that may give us a clue to the syndrome, being present. These include:
- Survivor of cardiac arrest
- Presence of polymorphic VT or VF
- History of non-vagal syncope
- Familial history of sudden death in less than 45 yo with no acute coronary syndrome
- Type I coved pattern in relatives
Other things to consider
Brugada Phenocopies
There are so called Brugada phenocopies, which are Brugada patterns arising from various causes which can include:
The only proven therapy for these patients is an implantable defibrillator.(6) In the acute setting, we need to discuss all these patients with cardiology. However only those patients with a typical ECG pattern and clinical criteria will need admission
Those with a type I pattern, should all be admitted as they have a significant risk of mortality. An incidental finding of this pattern does predict a lower risk of mortality.
There are so called Brugada phenocopies, which are Brugada patterns arising from various causes which can include:
- Metabolic disorders
- Electrocution
- Ischaemia
- Cardioversion, which usually resolve on resolution of the injury. Their prognosis is unknown.
- Supraventricular arrhythmias in Brugada
- 20% of patients with Brugada develop supraventricular arrhythmias.(5).Up to 20% of cases have atrial fibrillation. Atrioventricular nodal re-entry tachycardia and Wolff-Parkinson White Syndrome have also been described(5)
The only proven therapy for these patients is an implantable defibrillator.(6) In the acute setting, we need to discuss all these patients with cardiology. However only those patients with a typical ECG pattern and clinical criteria will need admission
Those with a type I pattern, should all be admitted as they have a significant risk of mortality. An incidental finding of this pattern does predict a lower risk of mortality.