Hypertensive emergencies are defined as sudden and prolonged increases in the arterial blood pressure, with associated organ damage. The degree of increase above that which the patient normally has, and the degree and duration of the rise are not usually taken into account.
No single figure for blood pressure is usually defined, however if a single figure was important, we should be concerned with readings of :
Rate of Blood Pressure reduction
As a general rule(ie not the exceptions below), blood pressure should be reduced by <25% within the first hour.
If the patient is stable further reduction can occur over the next 2-6 hours to:
Exceptions to Slow Blood Pressure reduction
In the following circumstances the blood pressure must be reduced rapidly
No single figure for blood pressure is usually defined, however if a single figure was important, we should be concerned with readings of :
- Systolic Blood Pressure > 180mmHg and /or
- Diastolic Blood Pressure > 120mmHg
Rate of Blood Pressure reduction
As a general rule(ie not the exceptions below), blood pressure should be reduced by <25% within the first hour.
If the patient is stable further reduction can occur over the next 2-6 hours to:
- Systolic blood pressure of 160mmHg
- Diastolic blood pressure of 100-110 mmHg
Exceptions to Slow Blood Pressure reduction
In the following circumstances the blood pressure must be reduced rapidly
- Aortic Dissection: Reduce the systolic blood pressure to < 120 mmHg within an hour and probably within 20 minutes
- Pre-eclampsia / Eclampsia/ Paeochromocytoma crisis: Reduce systolic blood pressure to <140mmHg within an hour
- Ischaemic stroke patients eligible for thrombolysis: Reduce systolic blood pressure <185 mmHg and diastolic blood pressure to <110mmHg
- Intracerebral bleeds have some specific requirements described below
What medications can we use?
There are multiple medications available, however I have included the most commonly used medications to make it simpler.
- Beta blocker
- 10-20mg IV to maximum dose of 300mg
- IV infusion at 0.5-2 mg/min
- Onset of action: 5-10 minutes
- Duration of action: 3-8 hours
- Contraindicated in the hypertensive patient in:
- asthma or obstructive airway disease,
- severe bradycardia,
- 2°/3° heart block (without pacemaker),
- Selective beta1-blocker, little effect on beta2 receptors unless high doses.
- 0.25-0.5 mg/kg IV over 1 min, then
- 0.05-0.3 mg/kg/min IV infusion
- Onset of action: 2-10 min (IV)
- Duration of action: 10-30 min
- Contraindicated in the hypertensive patient in:
- asthma or obstructive airway disease,
- severe bradycardia,
- 2°/3° heart block (without pacemaker),
- Direct vasodilator; dilates arterioles with little effect on veins; decreases systemic resistance
- 5-20mg IV bolus
- 0.5-10 mg/hr IV infusion
- Onset of action: 5-20 min
- Duration of action: 1-4 hr (IV)
- Contraindicated in
- Aortic dissection
- Ischaemic strokes
- Intracerebral haemorrhages
- Coronary artery disease
- Mitral valve rheumatic heart disease
- Organic nitrate: systemic venodilation, decreases preload
- 5-10mcg/min IV and titrate infusion
- Onset of action: 1-3 min
- Duration of action: 3-5 min
- 0.3 mcg/kg/min IV to a maximum of 10 mcg/kg/min
- Relaxes vascular smooth muscle, reduces afterload and preload
- Onset of action: <2 min
- Duration of action: 1-10 min
- Contraindicated
- Hypersensitivity
- Intracranial ischaemia/bleeds as increases intracranial pressure
- Pregnancy, as can cause cyanide toxicity
CASE 1. A 45 YO MALE WITH SUDDEN SEVERE CHEST PAIN
45 yo male with sudden onset severe chest pain + pain in upper back.
His BP is BP 165/90, although there is a BP difference between arms of >20mmHg
Given his history, you are concerned about an acute thoracic dissection.
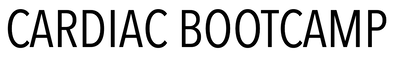
You perform a chest x-ray
There is an obvious widened mediastinum.
This fits with the clinical picture of a thoracic aortic dissection.
His BP is BP 165/90, although there is a BP difference between arms of >20mmHg
Given his history, you are concerned about an acute thoracic dissection.
You perform a chest x-ray
There is an obvious widened mediastinum.
This fits with the clinical picture of a thoracic aortic dissection.
Managment
- The aim of treatment is to decrease the blood pressure and the shear stress on the aorta, minimising the propagation of dissection.
- The systolic blood pressure should be lowered rapidly to < 120 mmHg. Beware not to overshoot with blood pressure control.
- Treatment is with a beta blocker such as Labetalol or esmolol
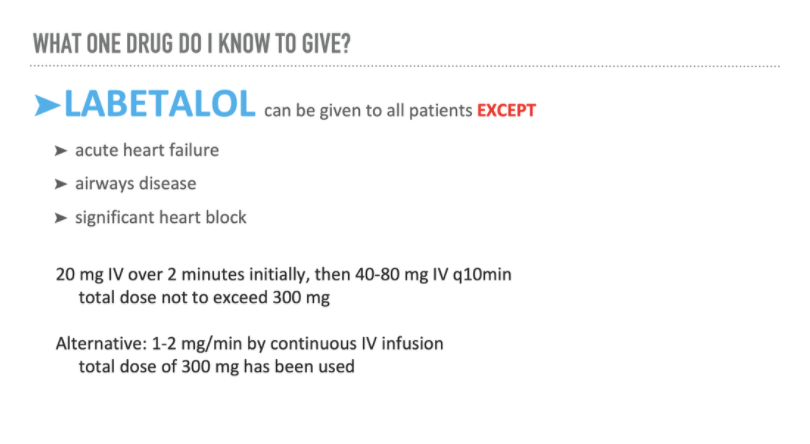
- If using Labetalol
- Blocks alpha 1 and beta
- Can be used for most hypertensive emergencies
- It doesn’t cause reflex tachycardia even though it is a vasodilator
- Contraindicated in:
- Airways disease
- Acute Heart Failure
- Hydralazine is contraindicated as it can increase the shear stress.
- If the blood pressure is not being controlled then Nitroprusside or Nitroglycerin can be added, but only after a beta blocker is used as these infusions can result in a reflex tachycardia.
If we look at lead
A Special Case
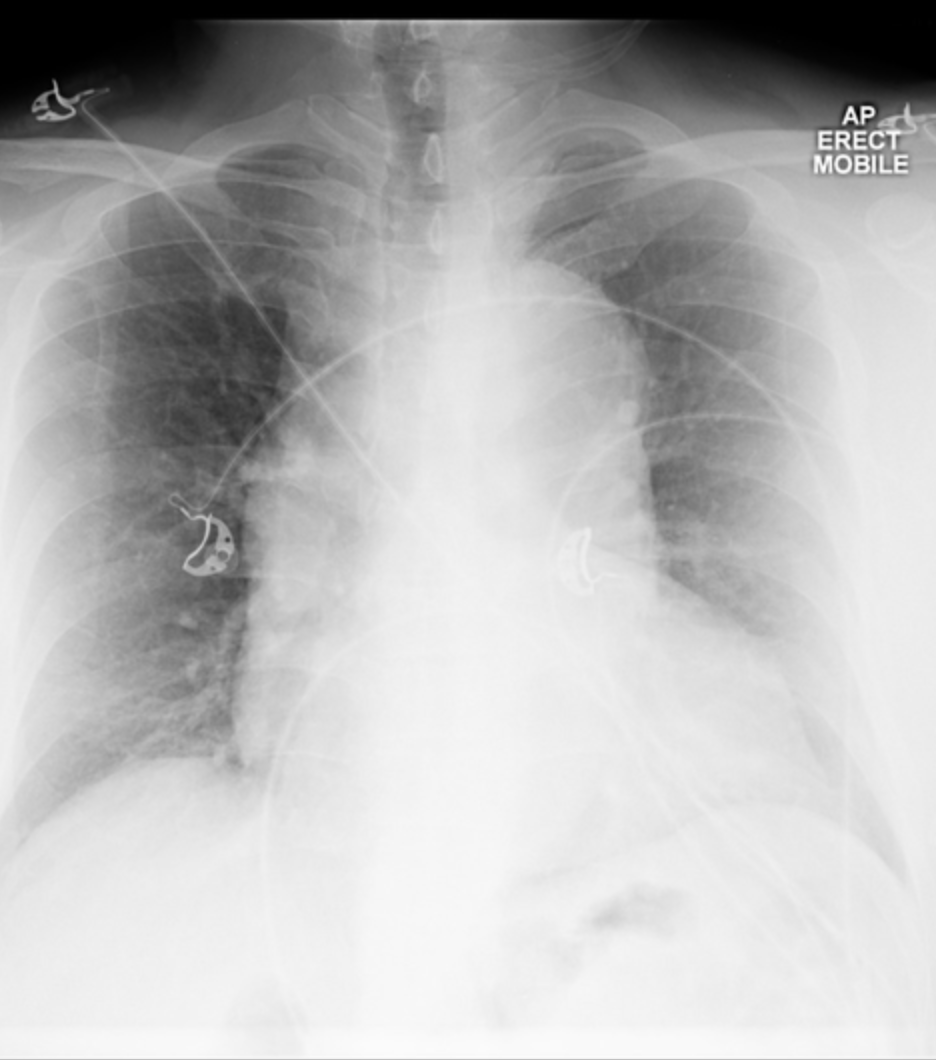
If in the above case of the 45 yo with a thoracic aortic dissection, you perform an ecg, which looks like the following. What is this?
If we look at leads V3-V6, we see large complexes, and there are T wave inversions. The T waves are in the form of ticks. This is a classic T wave of left ventricular hypertrophy.
To measure left ventricular hypertrophy, you can use any of the recognised criteria(see advanced ECG). HOWEVER, here is a quick way to tell. If the QRS of one anterior lead overlaps the QRS of another anterior lead, it's left ventricular hypertrophy.
This patient actually has a history of Hypetrophic Obstructive Cardiomyopathy (HOCM).
If we look at leads V3-V6, we see large complexes, and there are T wave inversions. The T waves are in the form of ticks. This is a classic T wave of left ventricular hypertrophy.
To measure left ventricular hypertrophy, you can use any of the recognised criteria(see advanced ECG). HOWEVER, here is a quick way to tell. If the QRS of one anterior lead overlaps the QRS of another anterior lead, it's left ventricular hypertrophy.
This patient actually has a history of Hypetrophic Obstructive Cardiomyopathy (HOCM).
How do you treat the patient with dissection and HOCM?
Labetalol is still the drug to use.
What if you have no labetalol in your hospital. Then consider esmolol.
What if you don't have that either?
Can you use GTN or Nitroprusside?
What if you have no labetalol in your hospital. Then consider esmolol.
What if you don't have that either?
Can you use GTN or Nitroprusside?
|
GTN INFUSION - BEWARE
|
NITROPRUSSIDE INFUSION
|
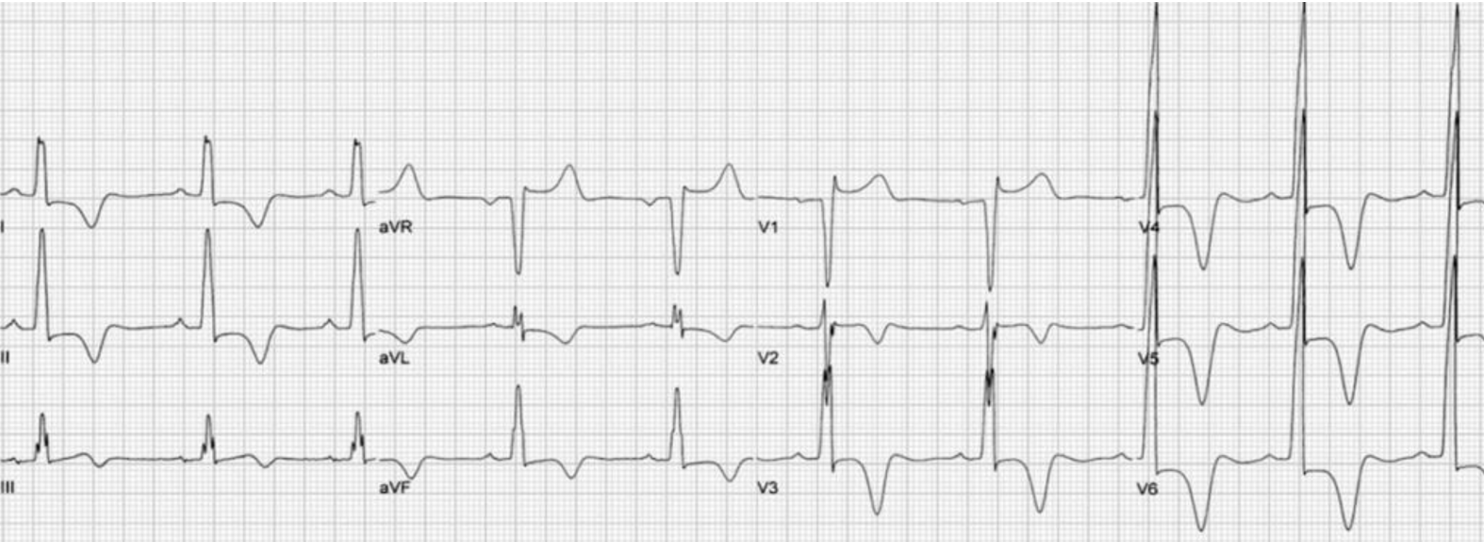
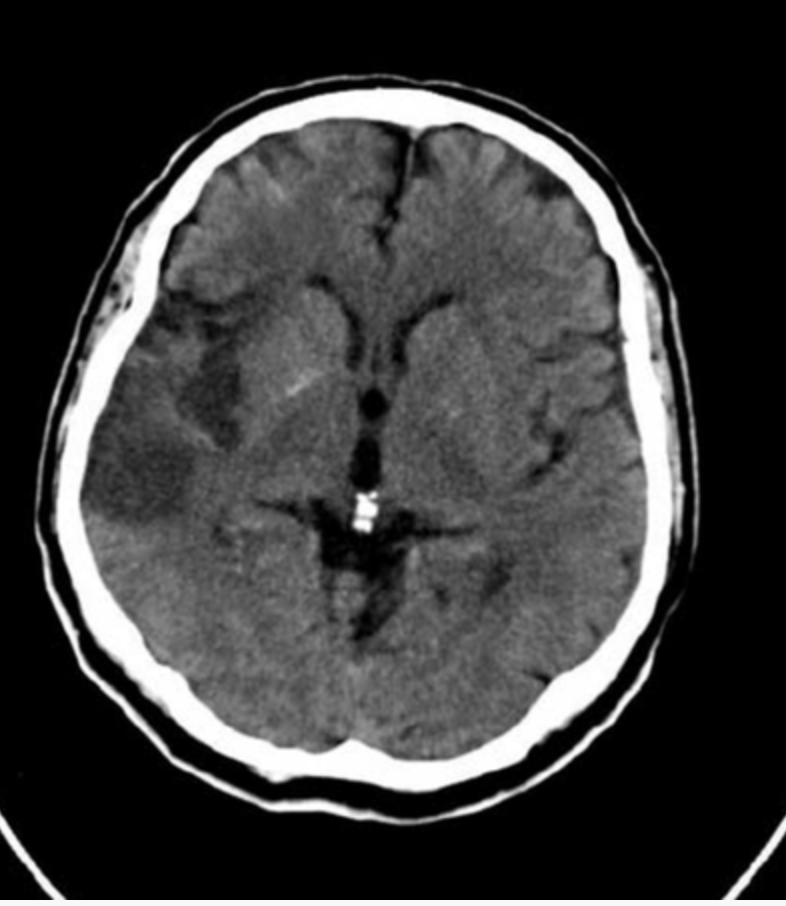
CASE 2. A 68 YO MALE PRESENTS WITH SUDDEN, SEVERE HEADACHE AND ARM WEAKNESS
MANAGING BLOOD PRESSURE IN ACUTE CEREBRAL HAEMORRHAGE
- Treatment is needed if the systolic blood pressure is > 220 mmHg
- There is controversy as to the lower limit of blood pressure. It is advised that care should be taken not to lower the systolic blood pressure to < 140 mmHg in those presenting in the first 6 hours, post bleed.
- Labetalol is the drug of choice.
- Avoid Nitroprusside and Hydralazine as they can increase intracranial pressure.
THE EVIDENCE
IntroductionThe ATACH-2 trial (Antihypertensive Treatment of Acute Cerebral Haemorrhage II) is an important trial in respect to the management of intracerebral bleeds.
We know that intra-cerebral bleeds are dynamic, with up to 40% of patients having growth in haemorrhage volume, in the first 3 hours(Stroke 1997:28:1-5). We also know that bleed volume is a determinant of mortality and that bleed volume increase, is related to increased blood pressure(Neurosurgery 1994). Because of this, there has been a push to lower systolic blood pressure(SBP) in acute bleeds. I am not including subarachnoid bleeds in this discussion.
Read the Penumbra Conundrum above were I point out that hemorrhagic strokes are very different to ischaemic strokes. Hemorrhagic strokes have no ischaemic penumbra around the haematoma. Cerebral blood flow slows in the region as does metabolic rate (Stroke 2013:44;620-6).
INTERACT-2 TrialThe INTERACT 2 trial(NEJM 2013: 368: 2355-2365) randomised over 2000 patients into two systolic blood pressure groups:
The original ATACH-I trial used Nicardipine to lower SBP safely down to 110-140 (Crit Care Med 2010;38:637-648).
ATACH-2 TRIALThe ATACH-2 Trial just released, was a randomised multi centre trial that recruited patients within 4.5 hours of symptom onset. The blood pressures were kept at one of two levels for 24 hours:
1000 patients were randomised equally into the two groups. The study was stopped early, short of its 1280 patient target, due to futility. There was no difference in survival or benefit between the 2 groups i.e.., the intense lowering of SBP group and the less aggressive group. There may have been some increase in renal adverse events (not statistically significant) in the first 7 days in the more aggressive group, however the clinical implications of these are unclear.
Both INTERACT -II and ATACH-2 show no benefit in lowering blood pressure in intra-cerebral bleeds.
So where to now? What about the patient with SBP of 220mmHg? The only evidence so far is a study by Kazui S et al(Stroke 1996:27:1783-7) showing that SBP > 220mmHg was directly related to haematoma enlargement.
The American Heart Association recommends 140mmHg. I stick to 140 as my goal for SBP in spontaneous intracerebral haemorrhage. If I get 140-160mmHg i’m happy. If I go below 140, I know that studies have shown no harm. I try to not have fluctuations, but keep it steady. It is also important to monitor the patient as the SBP is lowered. Some patients with chronic hypertension will have a right shift in their auto regulation curve and lowering their SBP may produce neurological symptoms. They should have a higher SBP titrated.
Which antihypertensive to use? Remember that the SBP increases due to an increase in systemic vascular resistance (SVR):
We know that intra-cerebral bleeds are dynamic, with up to 40% of patients having growth in haemorrhage volume, in the first 3 hours(Stroke 1997:28:1-5). We also know that bleed volume is a determinant of mortality and that bleed volume increase, is related to increased blood pressure(Neurosurgery 1994). Because of this, there has been a push to lower systolic blood pressure(SBP) in acute bleeds. I am not including subarachnoid bleeds in this discussion.
Read the Penumbra Conundrum above were I point out that hemorrhagic strokes are very different to ischaemic strokes. Hemorrhagic strokes have no ischaemic penumbra around the haematoma. Cerebral blood flow slows in the region as does metabolic rate (Stroke 2013:44;620-6).
INTERACT-2 TrialThe INTERACT 2 trial(NEJM 2013: 368: 2355-2365) randomised over 2000 patients into two systolic blood pressure groups:
- SBP < 140
- SBP <180
The original ATACH-I trial used Nicardipine to lower SBP safely down to 110-140 (Crit Care Med 2010;38:637-648).
ATACH-2 TRIALThe ATACH-2 Trial just released, was a randomised multi centre trial that recruited patients within 4.5 hours of symptom onset. The blood pressures were kept at one of two levels for 24 hours:
- 140-179 mmHg
- 110-139 mmHg
1000 patients were randomised equally into the two groups. The study was stopped early, short of its 1280 patient target, due to futility. There was no difference in survival or benefit between the 2 groups i.e.., the intense lowering of SBP group and the less aggressive group. There may have been some increase in renal adverse events (not statistically significant) in the first 7 days in the more aggressive group, however the clinical implications of these are unclear.
Both INTERACT -II and ATACH-2 show no benefit in lowering blood pressure in intra-cerebral bleeds.
So where to now? What about the patient with SBP of 220mmHg? The only evidence so far is a study by Kazui S et al(Stroke 1996:27:1783-7) showing that SBP > 220mmHg was directly related to haematoma enlargement.
The American Heart Association recommends 140mmHg. I stick to 140 as my goal for SBP in spontaneous intracerebral haemorrhage. If I get 140-160mmHg i’m happy. If I go below 140, I know that studies have shown no harm. I try to not have fluctuations, but keep it steady. It is also important to monitor the patient as the SBP is lowered. Some patients with chronic hypertension will have a right shift in their auto regulation curve and lowering their SBP may produce neurological symptoms. They should have a higher SBP titrated.
Which antihypertensive to use? Remember that the SBP increases due to an increase in systemic vascular resistance (SVR):
- Nicardipine (5mg/hr IV, increase every 5-10 min by 2.5mg/hr)
- Labetalol- 10-20mg bolus, every 15 minutes up to 300mg
- GTN infusion or
- Hydrazine 5 mg bolus IV and a hydrazine infusion.
How to Control Blood Pressure in Intracranial HaemorrhageThe scenario is this:
A 62 year old male is brought in to your emergency department by ambulance. He has had a sudden onset of headache and has decreased use of left side. His vitals are:
GCS 14, HR 92, BP 210/100, Sats 95% on room air. A CT reveals a large intracranial haemorrhage.
Do we lower the blood pressure? If yes, to what do we lower it to? What’s the evidence?
We know that a key determinant of outcome in hemorrhagic stroke is haematoma volume(Stroke 1997;28:1-5), so that a large haematoma, or haematoma expansion is associated with poor outcomes. We also know that intracerebral haemorrhage and associated high blood pressure, has a poor clinical outcome (JHypertension 2005;23:1217-23)
The first thing to make clear is that hemorrhagic stroke is different to ischaemic stroke. In ischaemic stroke, all the fuss related to lysis, is about perfusing and salvaging the penumbra of ischaemic brain tissue, surrounding the dead central tissue.
This penumbra doesn’t exist around hemorrhagic tissue. This region is said to be in a hibernating state and the low cerebral blood flow is matched by a low metabolic rate. CT perfusion scans show no adverse effect on perihaematoma blood flow, with early aggressive BP control to a systolic of less than 150mmHg (Stroke 2013;44:620-26)
What should we lower the blood pressure to?The INTERACT 2 trial (NEJM 2013;368:2355-65) is the largest randomised trial of patients with intracerebral haemorrhage and blood pressures up to 220mmHg, where control was within 6 hours, to two systolic blood pressure groups:
1. <140mmHg
2. <180mmHg
Overall the trial did not show a reduction in death or disability, although there was a trend towards improved functional outcomes in the <140mmHg group.
What is also important is that the group with aggressive blood pressure control to < 140mmHg did not show early neurologic deterioration or adverse events. What it did show, was a lower haematoma volume.
The ATTACH Trial was interesting from this point of view as it had similar arms, but also a third arm that looked at aggressive BP control i.e.., 110-140mmHg. Again, no adverse events with aggressive blood pressure lowering.
Only one study has ever shown poor outcome from aggressive blood pressure lowering to 140mmHg (J Intern Med. 2004;255:257–265)
What about subarachnoid haemorrhage?Not much great evidence here. We know that rebleeding with potentially catastrophic effects can occur in the first 12 hours. This rebleeding is strongly associated with hypertension ie., systolic blood pressure >160mmHg (Arch Neurol.2005;62:410-416). Most recommendations here are consensus opinion.
What do you use to lower blood pressure in intracranial haemorrhage?Aim for short acting, easily titratable and something that doesn’t affect cerebral blood flow.
What would you use for the initial lowering of BP?
(a) Labetalol
(b) GTN infusion
(c) Sodium Nitroprusside
(d) Hydralazine
(e) Nicardipine
I would probably opt for Labetalol 10-20mg bolus every 10-15minutes
If I had Nicardipine, I may opt for that as a first line agent at 1-2mg/hour as an infusion, doubling it every few minutes to a maximum of 16mg/hr. I like this, because of its short half life of 5-10 minutes.
Beware GTN infusion and Sodium Nitroprusside as they can affect cerebral blood flow.
Hydralazine lowers blood pressure very effectively, with an onset at 3-5 minutes. One of it’s side effects is that it increases intracranial pressure (Stroke. 1975;6:402-404), as a balance to this, it also increases cerebral blood flow.
A 62 year old male is brought in to your emergency department by ambulance. He has had a sudden onset of headache and has decreased use of left side. His vitals are:
GCS 14, HR 92, BP 210/100, Sats 95% on room air. A CT reveals a large intracranial haemorrhage.
Do we lower the blood pressure? If yes, to what do we lower it to? What’s the evidence?
We know that a key determinant of outcome in hemorrhagic stroke is haematoma volume(Stroke 1997;28:1-5), so that a large haematoma, or haematoma expansion is associated with poor outcomes. We also know that intracerebral haemorrhage and associated high blood pressure, has a poor clinical outcome (JHypertension 2005;23:1217-23)
The first thing to make clear is that hemorrhagic stroke is different to ischaemic stroke. In ischaemic stroke, all the fuss related to lysis, is about perfusing and salvaging the penumbra of ischaemic brain tissue, surrounding the dead central tissue.
This penumbra doesn’t exist around hemorrhagic tissue. This region is said to be in a hibernating state and the low cerebral blood flow is matched by a low metabolic rate. CT perfusion scans show no adverse effect on perihaematoma blood flow, with early aggressive BP control to a systolic of less than 150mmHg (Stroke 2013;44:620-26)
What should we lower the blood pressure to?The INTERACT 2 trial (NEJM 2013;368:2355-65) is the largest randomised trial of patients with intracerebral haemorrhage and blood pressures up to 220mmHg, where control was within 6 hours, to two systolic blood pressure groups:
1. <140mmHg
2. <180mmHg
Overall the trial did not show a reduction in death or disability, although there was a trend towards improved functional outcomes in the <140mmHg group.
What is also important is that the group with aggressive blood pressure control to < 140mmHg did not show early neurologic deterioration or adverse events. What it did show, was a lower haematoma volume.
The ATTACH Trial was interesting from this point of view as it had similar arms, but also a third arm that looked at aggressive BP control i.e.., 110-140mmHg. Again, no adverse events with aggressive blood pressure lowering.
Only one study has ever shown poor outcome from aggressive blood pressure lowering to 140mmHg (J Intern Med. 2004;255:257–265)
What about subarachnoid haemorrhage?Not much great evidence here. We know that rebleeding with potentially catastrophic effects can occur in the first 12 hours. This rebleeding is strongly associated with hypertension ie., systolic blood pressure >160mmHg (Arch Neurol.2005;62:410-416). Most recommendations here are consensus opinion.
What do you use to lower blood pressure in intracranial haemorrhage?Aim for short acting, easily titratable and something that doesn’t affect cerebral blood flow.
What would you use for the initial lowering of BP?
(a) Labetalol
(b) GTN infusion
(c) Sodium Nitroprusside
(d) Hydralazine
(e) Nicardipine
I would probably opt for Labetalol 10-20mg bolus every 10-15minutes
If I had Nicardipine, I may opt for that as a first line agent at 1-2mg/hour as an infusion, doubling it every few minutes to a maximum of 16mg/hr. I like this, because of its short half life of 5-10 minutes.
Beware GTN infusion and Sodium Nitroprusside as they can affect cerebral blood flow.
Hydralazine lowers blood pressure very effectively, with an onset at 3-5 minutes. One of it’s side effects is that it increases intracranial pressure (Stroke. 1975;6:402-404), as a balance to this, it also increases cerebral blood flow.
CASE 3. A 68 YO MALE PRESENTS WITH SEVERE HEADACHE AND ARM WEAKNESS
SHOULD WE TREAT THE BLOOD PRESSURE?
In making the decision, a critical question to ask is:
IS THE PATIENT SUITABLE FOR THROMBOLYSIS?
IS THE PATIENT SUITABLE FOR THROMBOLYSIS?
- If the answer is YES, then w need to treat the BP if it > 185/110
- If the answer is NO, then do not treat it unless it is > 220/120
MANAGEMENT
- In an ischaemic stroke, where no treatment is planned, blood pressure doesn’t need to be lowered unless the systolic blood pressure is >220 mmHg or the diastolic blood pressure is > 120 mmHg. At these levels consideration can be given to lowering of the blood pressure. Beware that the blood pressure decrease, doesn’t cause further ischaemia.
- Treatment is needed if the patient is due for thrombolysis. The aim is:
- Systolic blood pressure of <185mmHg
- Diastolic blood pressure of <110 mmHg
- Labetalol is the drug of choice.
- Avoid Nitroprusside and Hydralazine as they can increase intracranial pressure
We've look at the intracranial bleed and ischaemia
What about Subarachnoid Haemorrhage?
- Aim to keep the systolic blood pressure < 160 mmHg
- Beta blockers such as Labetalol and Esmolol are the drugs of choice here.
- Avoid Nitroprusside and Hydralazine as they increase intracranial pressure
CASE 4. A 38 YO WOMAN WHO IS 9 DAYS POST PARTUM
This 38 yo woman is due to have her sutures removed from her caesarean section wound today.
She is headed for clinic, however she comes to the emergency department prior as she has had a headache all day.
Her vitals are normal except for her BP being 168/90.
Is this of concern?
- Hypertension of any reading in 20 weeks gestation to 2 weeks post partum is of concern: think preeclampsia
- Pre-eclampsia is associated with high maternal and fetal morbidity and mortality
- A BP > 140/90 in previously healthy, we should worry
MANAGEMENT
- Lower the systolic blood pressure to < 140mmHg within the first hour
- Labetalol and Hydralazine are the agents of choice
- There may be some concern with Hydralazine in terms of neonatal effects
- Avoid Nitroprusside due to the potential for fetal cyanide poisoning
- ACE inhibitors, Angiotensin receptor blockers are avoided due to teratogenic effects
CASE 5. A 27 YO MALE PRESENTS AGITATED AND TACHYCARDIC WITH A BP OF 190/125
He admits to having taken cocaine.
WHAT MUST YOU BEWARE OF IN THIS PATIENT?
BEWARE
Beta blockers are CONTRAINDICATED, as they may make the patients heart rate and BP even worse due to blocking beta receptors, resulting in unopposed alpha activity.
Benzodiazepines are the treatment of choice.
Beta blockers are CONTRAINDICATED, as they may make the patients heart rate and BP even worse due to blocking beta receptors, resulting in unopposed alpha activity.
Benzodiazepines are the treatment of choice.
- Hyperadrenergic states can occur following cocaine or amphetamine use, or in those patients with a pheochromocytoma
- First line agents when sympathomimetic drugs are used are benzodiazepines
- If first line agents don’t work, consider phentolamine (alpha adrenergic blocker)
- A beta blocker alone is contraindicated as it will result in unopposed alpha adrenergic vasoconstriction, resulting in further blood pressure increase.
Other Conditions
Myocardial Ischaemia/Infarction
Left Ventricular Failure and /or Pulmonary Oedema
- Treatment may be commenced if:
- Systolic blood pressure is >160 mmHg and/or
- Diastolic blood pressure is >100 mmHg
- Treatment is with a beta blocker (Labetalol or Esmolol) and Nitroglycerin
Left Ventricular Failure and /or Pulmonary Oedema
- Aim to keep the blood pressure < 130/80
- Nitroglycerin is the first line drug
- Nitroprusside is a second line drug
- Consider a loop diuretic such as frusemide
- Beware, as beta blockers are contraindicated
SUPER SUMMARY
In these two condition, it can be decreased much more rapidly and certainly within the first hour.
If there is one medication to know well it is:
If there is one medication to know well it is:
Please answer the following questions:
QUESTION 1: IN A PATIENT WITH A SUSPECTED THORACIC AORTIC DISSECTION, THE BLOOD PRESSURE MUST BE REDUCED RAPIDLY TO A SYSTOLIC OF <120MMHG. TRUE OR FALSE?
ANSWER
True
QUESTION 2: IN A PATIENT WHO IS 32 WEEKS GESTATION AND HAS A BP OF >140/90, THE BP CAN BE REDUCED TO NORMAL LEVELS RAPIDLY. TRUE OR FALSE?
ANSWER
True
QUESTION 3: LABETALOL CAN BE USED TO TREAT ALL CASES OF SEVERE HYPERTENSION. TRUE OR FALSE ?
answer
FALSE:
They cannot be used in those patients with a hyperadrenergic state such
They cannot be used in those patients with a hyperadrenergic state such
- Cocaine or Amphetamines
- Those with a pheochromocytoma
- Airways Disease
- Acute heart Failure and
- Significant Heart Block