A 60 yo male collapses at work
A 60 yo male is brought into the Emergency Department following collapsing at work.
On arrival he is alert and oriented with a heart rate of 20bpm, BP of 105/70 and a respiratory rate of 16.
He has no chest pain or other concerning features.
His past history includes:
(a) Increase his heart rate using pharmacology
(b) Do nothing as you might cause harm and his blood pressure is acceptable and he is alert.
(c) Defibrillate
(d) Give Magnesium or an extra dose of Sotalol
On arrival he is alert and oriented with a heart rate of 20bpm, BP of 105/70 and a respiratory rate of 16.
He has no chest pain or other concerning features.
His past history includes:
- Atrial Fibrillation (on Sotalol and a NOAC)
- Hypercholesterolaemia
(a) Increase his heart rate using pharmacology
(b) Do nothing as you might cause harm and his blood pressure is acceptable and he is alert.
(c) Defibrillate
(d) Give Magnesium or an extra dose of Sotalol
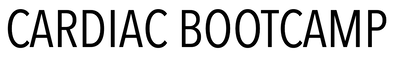
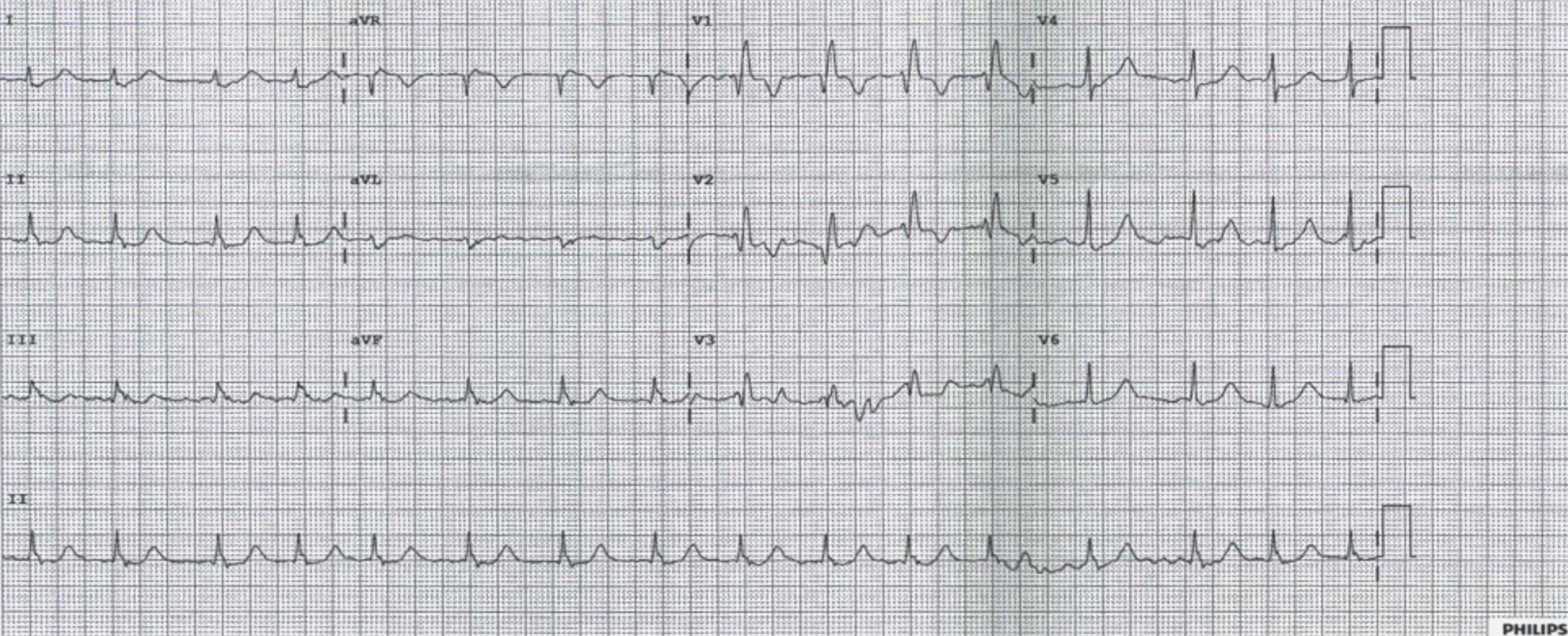
The ECG shows a slow regular (junctional) rhythm with narrow complexes and a RBBB.
Beware assuming that this patient's cardiac output is fine, given that he is alert and his blood pressure is 'acceptable'. The cardiac output MUST be reduced. CO = HR x SV The only reason the blood pressure is not low is due to a sympathetic response mounted by the patients, resulting in increased vasoconstriction.
(a) Increase his heart rate using pharmacology- The only real answer
(b) Do nothing as you might cause harm and his BP is acceptable and he is alert. X the patients cardiac output is reduced and they are only perfusing due to endogenous sympathetic response.
(c) Defibrillate X
(d) Give Magnesium or an extra dose of Sotalol X
Beware assuming that this patient's cardiac output is fine, given that he is alert and his blood pressure is 'acceptable'. The cardiac output MUST be reduced. CO = HR x SV The only reason the blood pressure is not low is due to a sympathetic response mounted by the patients, resulting in increased vasoconstriction.
(a) Increase his heart rate using pharmacology- The only real answer
(b) Do nothing as you might cause harm and his BP is acceptable and he is alert. X the patients cardiac output is reduced and they are only perfusing due to endogenous sympathetic response.
(c) Defibrillate X
(d) Give Magnesium or an extra dose of Sotalol X
Pharmacological Increase in Heart Rate
ATROPINE
Muscurinic Acetylcholine Receptor Antagonist
t1/2 = 3-4 hours
Indication: AV nodal blockade. It works by decreasing vagal tone, so may not be effective in high degree AVN block.
Dose: Start at 0.5 mg-1mg (max of 3mg) Lower doses may cause a reflex bradycardia
Beware:
Muscurinic Acetylcholine Receptor Antagonist
t1/2 = 3-4 hours
Indication: AV nodal blockade. It works by decreasing vagal tone, so may not be effective in high degree AVN block.
Dose: Start at 0.5 mg-1mg (max of 3mg) Lower doses may cause a reflex bradycardia
Beware:
- Patients with coronary artery disease as can increase myocardial demand
- Acute angle closure glaucoma
- Bowel obstruction
- Cardiac transplant patients- may result in asystole.
ISOPRENALINE
Beta adrenoreceptor agonist
t1/2 = 5 minutes, but immediate onset of action
Dose: If given centrally start at 0.5-1 mcg/min and titrate. It is also safe for peripheral infusion and can be started at 5mcg/min then titrate up or down. Usual range is 2-10 mag/min, however higher doses have been used.
Beware: Hypotension, tachycardia, angina. May not be tolerated by the patient longer term as can cause headaches and trembling.
Beta adrenoreceptor agonist
t1/2 = 5 minutes, but immediate onset of action
Dose: If given centrally start at 0.5-1 mcg/min and titrate. It is also safe for peripheral infusion and can be started at 5mcg/min then titrate up or down. Usual range is 2-10 mag/min, however higher doses have been used.
Beware: Hypotension, tachycardia, angina. May not be tolerated by the patient longer term as can cause headaches and trembling.
ADRENALINE
Non-selective adrenergic agonist Beta 1 > alpha 1 and Beta 2
t1/2 = 5 minutes. Acts within a minute and lasts for 5-10 minutes.
Dose: This can be used peripherally. Start dose at 1 mcg/min. Usual dose is 1-10 mcg/min. Higher doses may be needed.
It has a wide range of effect, being a chronotrope and inotrope.
Beware: Tachycardia and arrhythmias, narrow angle glaucoma, Phaeochromocytoma
Non-selective adrenergic agonist Beta 1 > alpha 1 and Beta 2
t1/2 = 5 minutes. Acts within a minute and lasts for 5-10 minutes.
Dose: This can be used peripherally. Start dose at 1 mcg/min. Usual dose is 1-10 mcg/min. Higher doses may be needed.
It has a wide range of effect, being a chronotrope and inotrope.
Beware: Tachycardia and arrhythmias, narrow angle glaucoma, Phaeochromocytoma
There are other pharmacological approaches you can use, such as Dopamine, Dobutamine, and even Calcium. However, if there has been no result with adrenaline, the next step is is to use pacing; either transcutaneous or transvenous pacing.
Mechanical Increase in Heart Rate
Transcutaneous Pacing
This is a simple and rapid procedure and is used when there is failure to increase the heart rate using pharmacological means. The procedure itself, although rapid, is a temporary solution until more definitive care is given, either by a temporary trans-venous pacemaker until pacemaker, or straight to pacemaker placement.
The usual approach to transcutaneous pacing is:
This is a simple and rapid procedure and is used when there is failure to increase the heart rate using pharmacological means. The procedure itself, although rapid, is a temporary solution until more definitive care is given, either by a temporary trans-venous pacemaker until pacemaker, or straight to pacemaker placement.
The usual approach to transcutaneous pacing is:
- Place pads in the AP position
- Use 'pacer' mode on the defibrillator pack.
- Set rate to 70 bpm
- Increase current from 0mA by 10mA at a time, until capture occurs.
- This is usually at 70-80mA. Set the current at 10mA above this
- If capture is not reached at above 110mA, reposition the pads and restart the process.
- Make sure that the capture is real- ie., time with the pulse or the arterial waveform on pulse oximetry.
Transvenous Pacing
Indications
The aim is to place the catheter into the right internal jugular vein. If this is not possible, the left subclavian may be used. The aim is to pass the pacing wire into the right ventricle. These two routes provide the most direct path.
Equipment
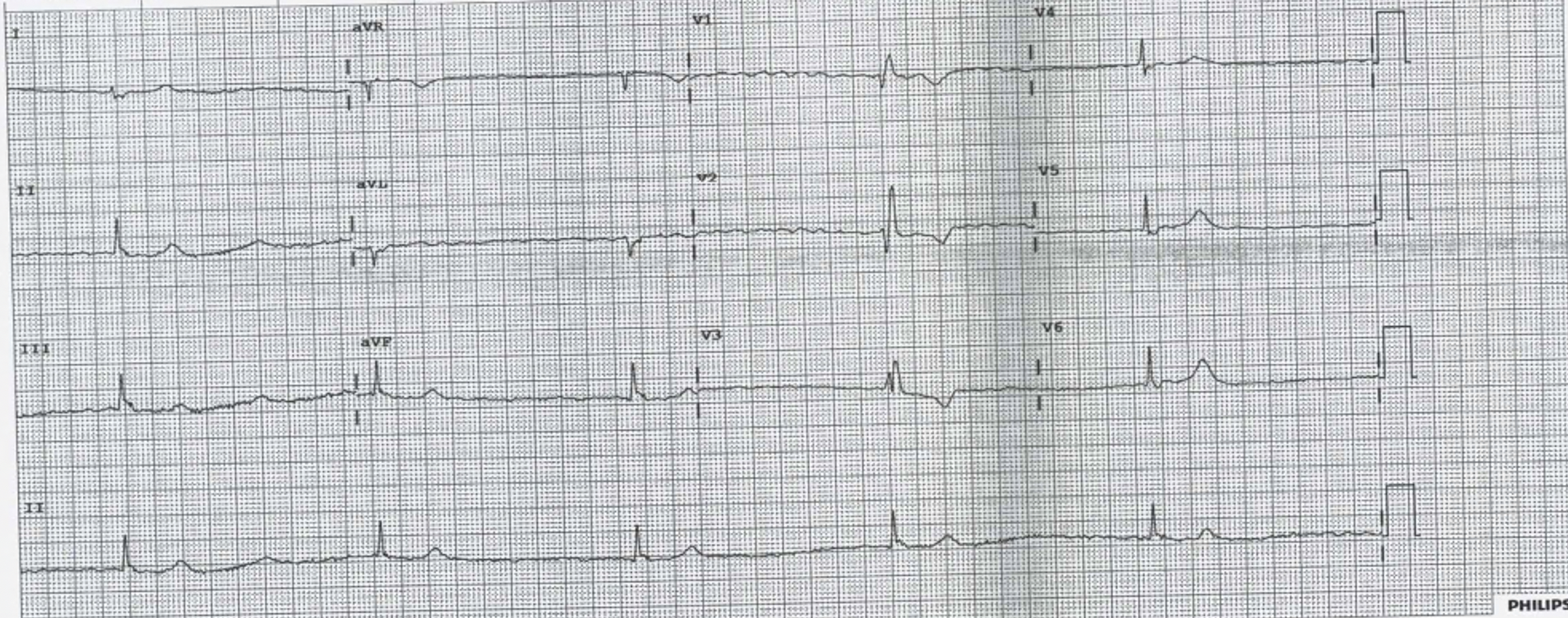
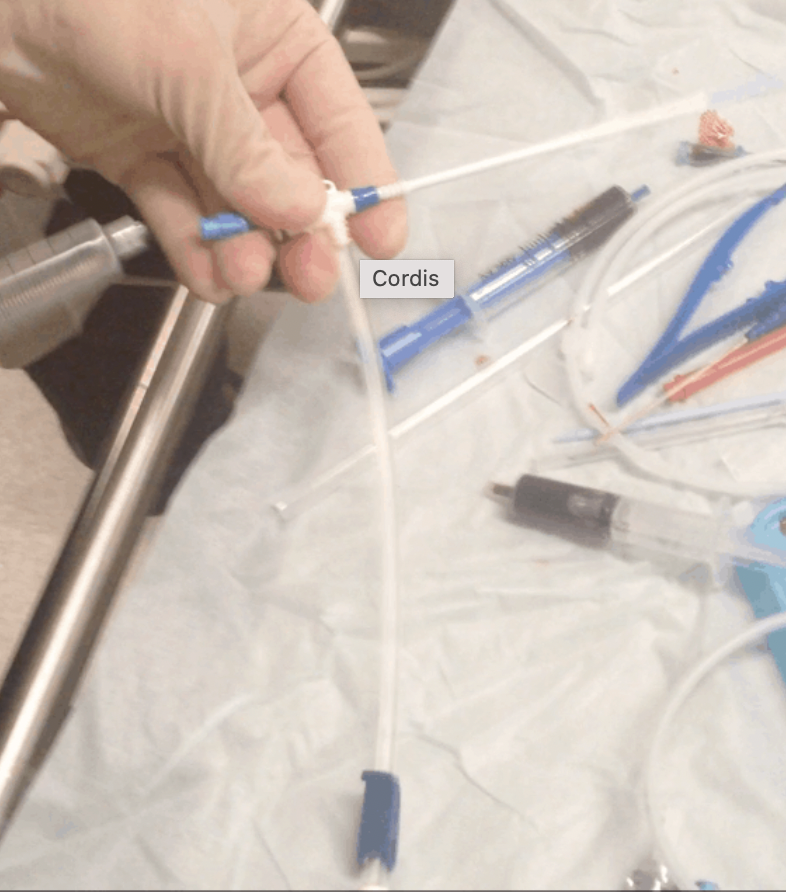
Use a central line kit to insert a guide wire into the right internal jugular vein. Ultrasound can be used to help here. The Cordis is a right angled set of tubing shown below. It is basically a wider sheath with a side port that can be used to inject.
Indications
- Patient not tolerating transcutaneous pacing
- Transcutaneous not actively capturing
- Unstable and needing transfer
The aim is to place the catheter into the right internal jugular vein. If this is not possible, the left subclavian may be used. The aim is to pass the pacing wire into the right ventricle. These two routes provide the most direct path.
Equipment
- A Cordis 6 french catheter. It has a balloon on the end and a single side port for medications
- The pacer catheter
- A Pacer sheath
- The pacer box
- A central line kit
Use a central line kit to insert a guide wire into the right internal jugular vein. Ultrasound can be used to help here. The Cordis is a right angled set of tubing shown below. It is basically a wider sheath with a side port that can be used to inject.
Using a Seldinger technique, feed the cordis over the guide wire. As you can see there is a dilator(blue end at the top of the cordis already in place, but a small cut to the skin may be needed to allow it to pass. When in position, the dilator which is part of the cordis can be removed and the catheter left in place. Blood will not come back up the catheter as it has an inbuilt diaphragm. You are now ready to put the pacing wire in. The temporary pacing wire comes in a pack separately. With it come two black electrodes at the end of the wire and in this case two yellow electrodes that fit into these black electrodes and then to the generator box.
|
Put the sheath over the pacer before putting it into the cords.However in this case the wire can be passed through the sheath
You can pass the pacing wire blind through the cordis to a length of 15 cm. You should now be in the central venous system. Inflate the balloon with 1.5ml of air and lock it. The balloon will stay up whilst the pacing wire is being placed in the right location. The balloon assists by moving towards the heart with the flow of blood. Ultrasound may be used very effectively here to see the wire passing into the right position. A second person should set up the pulse generator. Some have a preset emergency setting. If not start at a heart rate of 80 beats per minute and current of 20mA. With the generator come two black electrical ports and two red/yellow adaptors. The red/yellow adaptors slide into the black ports. The pacing catheter has 2 wires. The shorter inserts into the positive port, the longer wire into the negative. |
|
The aim is to have the tip of the wire at the apex of the right ventricle. This is where ultrasound is great.
When capture is achieved, deflate the balloon, but leave the syringe attached. Ensure the sheath covers the pacer wire and is locked. Suture the cordis into place. Adjust the current down so that capture is achieved… and voila! |
What happened to the patient?
He responded well to Isoprenaline..perhaps too well, becoming a little tachycardia. However given that isoprenaline has such a rapid turnoff effect, it was weaned. The patient was discussed with cardiology and was referred for a pacemaker.