What do we need to know? |
Narrow complex tachycardias are going to be sinus rhythm or an SVT.
Let's look at some types of narrow complex tachycardias.
Let's look at some types of narrow complex tachycardias.
AN NODAL RE-ENTRY TACHYCARDIA(AVNRT)
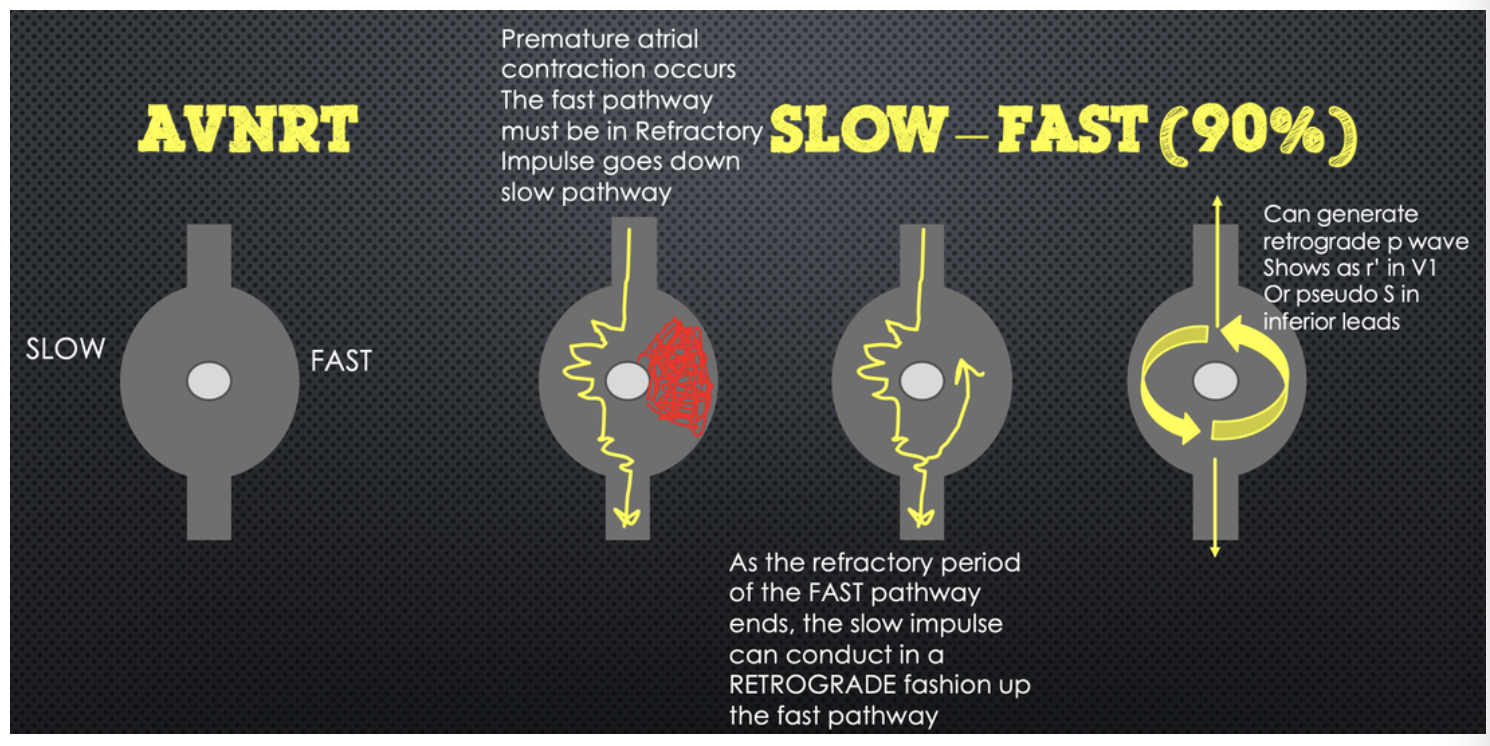
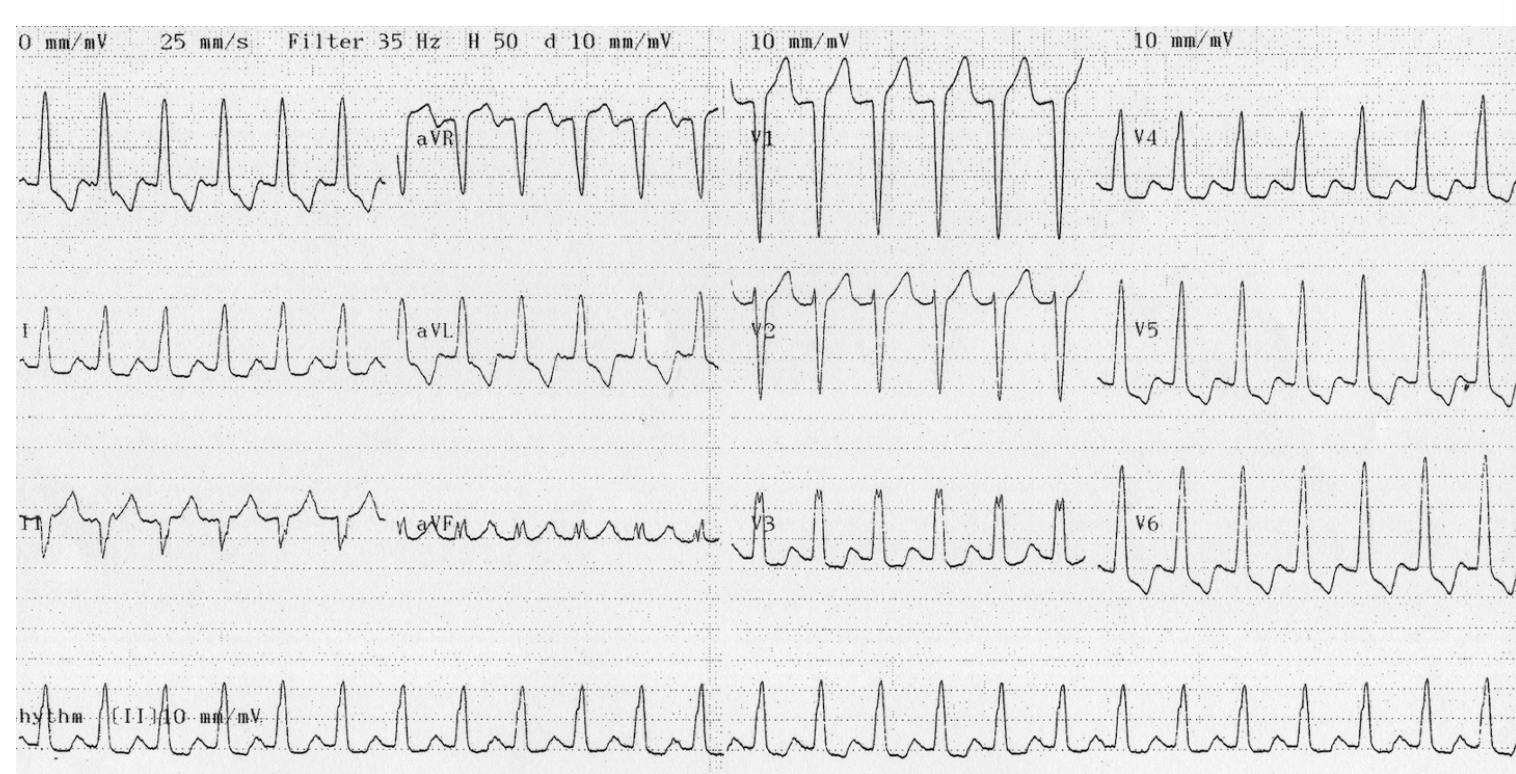
Look at the ECG below. The heart rate is about 200bpm. Are you concerned about the ST elevation in aVR?

This is a supraventricular tachycardia.(SVT)
ST elevation in aVR is part of SVT. It is not ischaemic. SVT's are not ischaemic. They can lead to ischaemia in a patient with coronary artery disease, if left for a period of time. However in themselves they are not ischaemic.
They are the commonest cause of palpitations + NO structural heart disease.
They occur due to a re-entry circuit within the atrioventricular node (AVN) formed by 2 pathways.
ST elevation in aVR is part of SVT. It is not ischaemic. SVT's are not ischaemic. They can lead to ischaemia in a patient with coronary artery disease, if left for a period of time. However in themselves they are not ischaemic.
They are the commonest cause of palpitations + NO structural heart disease.
They occur due to a re-entry circuit within the atrioventricular node (AVN) formed by 2 pathways.
- A slow pathway
- A fast pathway
- One allows fast conduction and thus has a long refractory period.
- The other allows slow conduction and thus has a short refractory period.
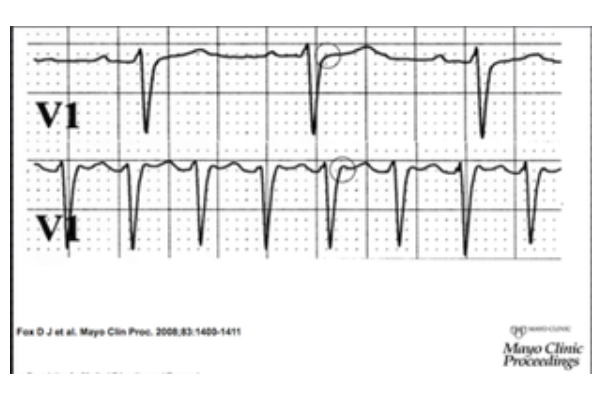
The SLOW-FAST Pathway (90%) of cases
|
For the SLOW-FAST pathway, to be activated, a premature atrial contraction occurs and travels down the SLOW arm. The FAST pathway must be in the refractory period.. As this refractory period ends the impulse traveling down the SLOW pathway conducts retrogradely into the FAST pathway. This generates a circus movement.
The result is that we will see an r1 in V1. |
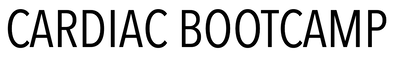
The FAST-SLOW Pathway (10%)
The opposite occurs. Fast conduction occurs down the FAST pathway and there is retrograde SLOW conduction.
This results in the P WAVE BEING SEEN AFTER THE QRS.
This results in the P WAVE BEING SEEN AFTER THE QRS.
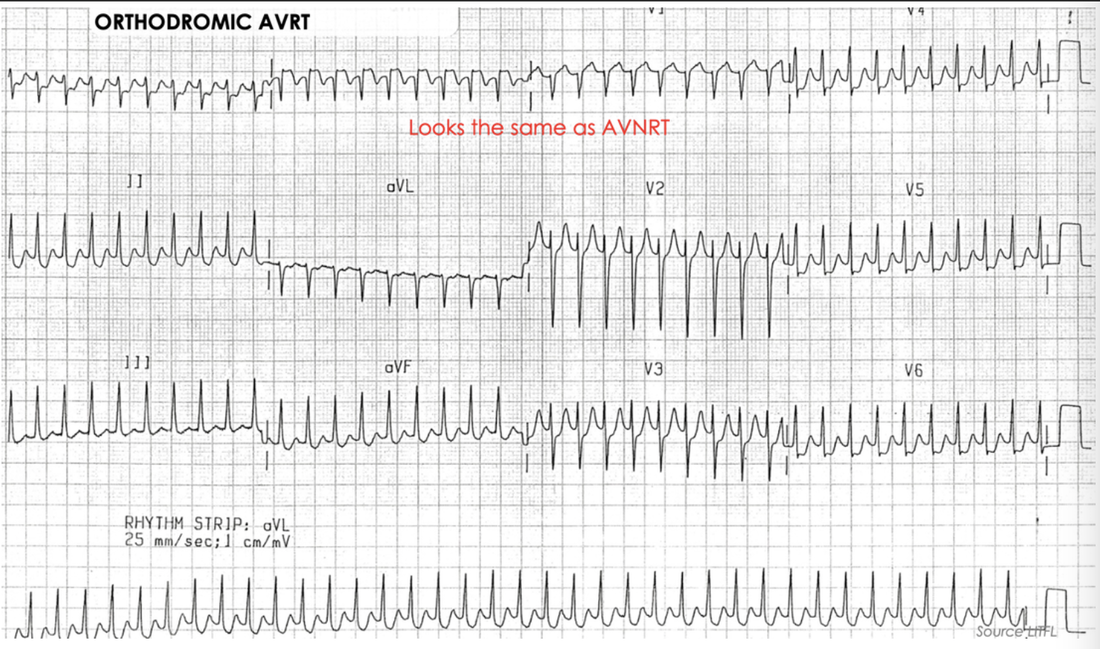
ATRIOVENTRICULAR RE-ENTRY TACHYCARDIA (AVRT)

We may not be able to distinguish it from AVNRT. In most cases it is ORTHODROMIC(95%)
This tachycardia involves an ACCESSORY PATHWAY. However there is no pre-excitation as the accessory pathway is part of the re-entry circuit.
This tachycardia involves an ACCESSORY PATHWAY. However there is no pre-excitation as the accessory pathway is part of the re-entry circuit.
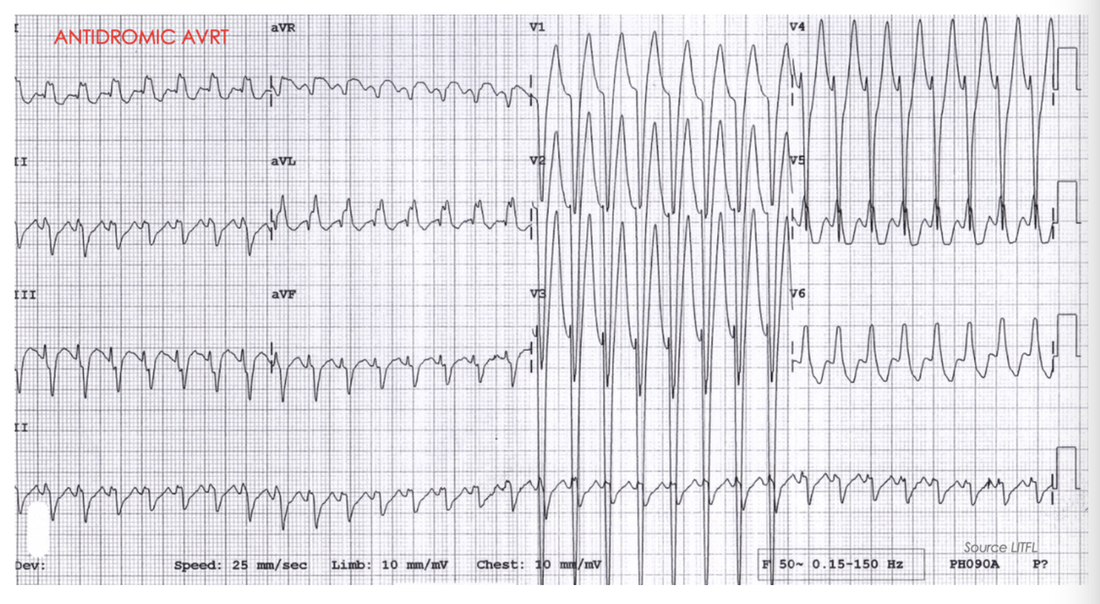
When ANTIDROMIC, the complexes are wide. The accessory pathway may be LEFT or RIGHT sided.
HOW TO TREAT NARROW COMPLEX TACHYCARDIAS.
REGULAR NARROW COMPLEX TACHYCARDIA can be treated with:
- Vagal manoeuvres
- Adenosine
- Electricity
|
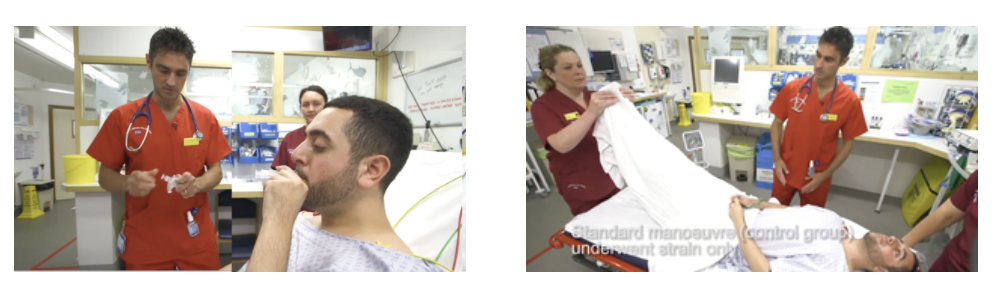
The REVERT trial
This was a randomised control trial of 433 patients . Normal SVT reversion rates with vagal manoeuvres is 20%. The REVERT trial reversion rate was 43% compared to 17% in their control group. What to do:
|
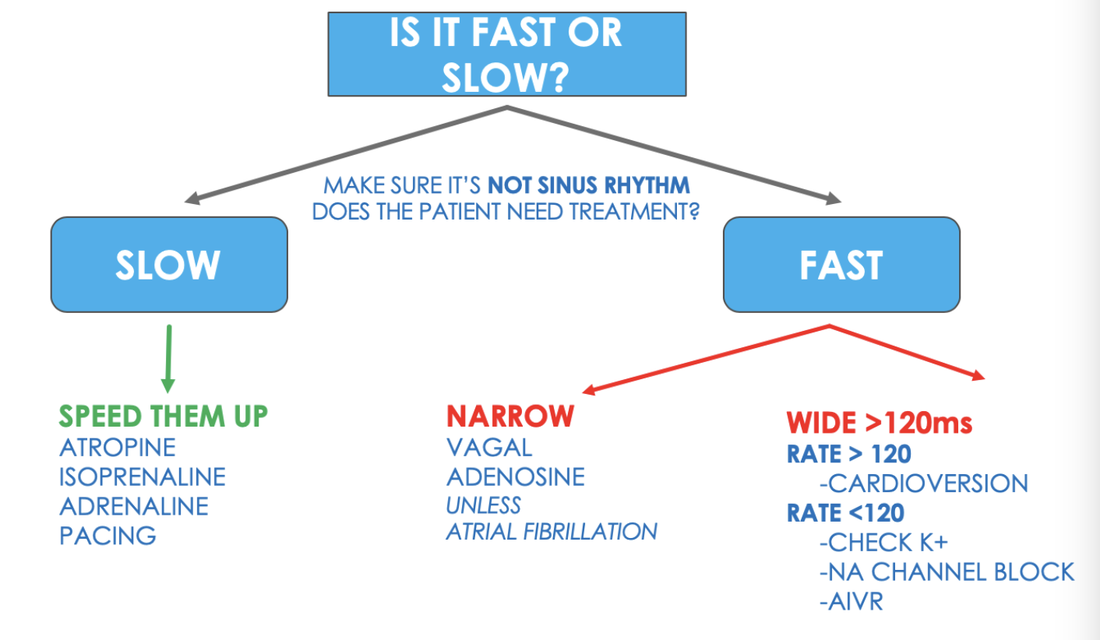
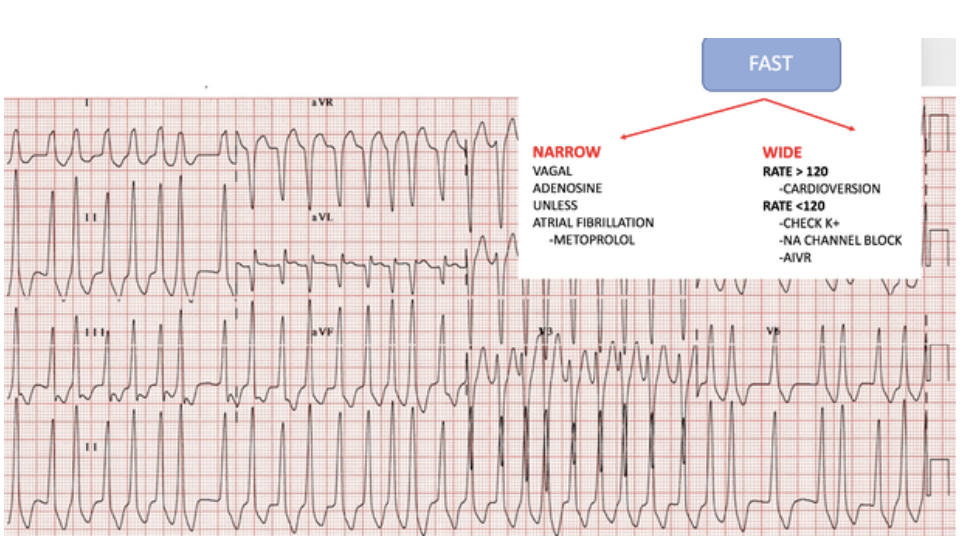
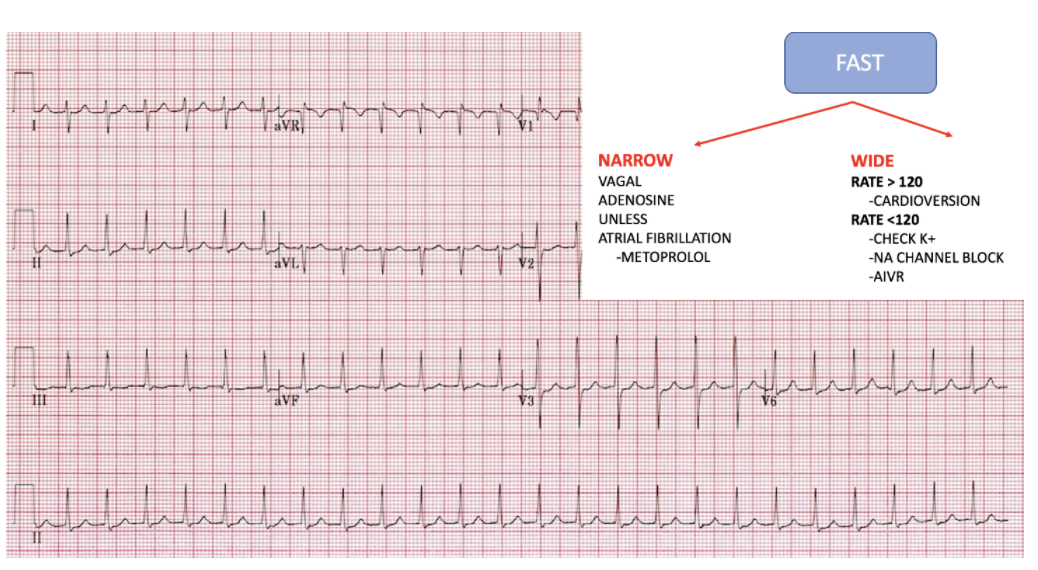
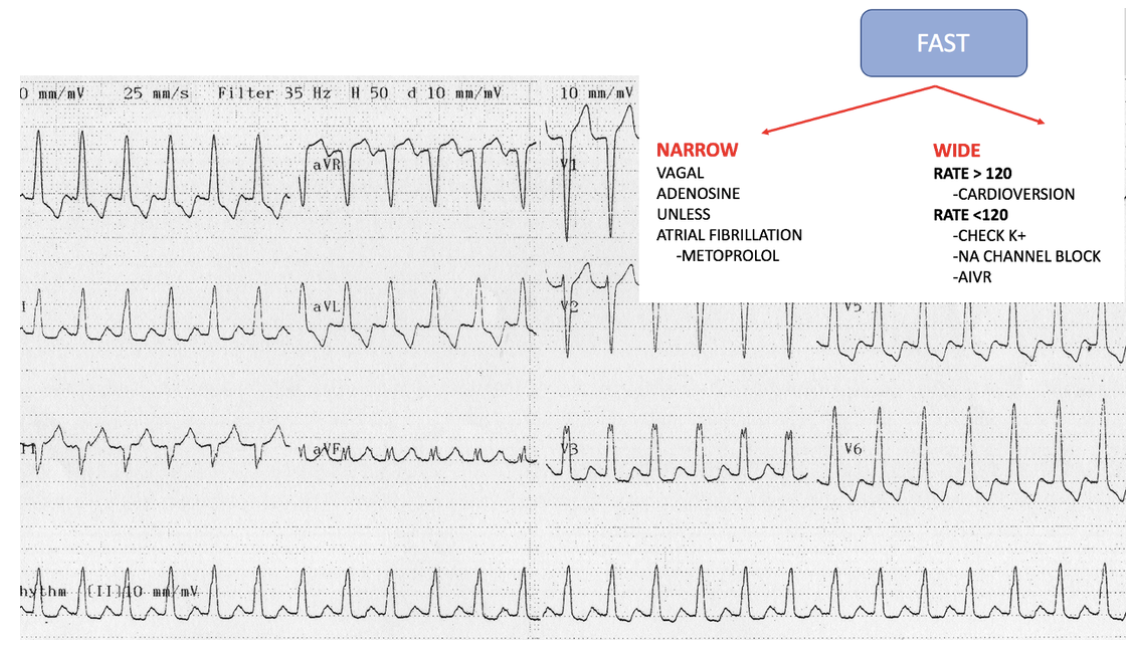
My Approach to Treatment
This is a simple approach, that maximises results and minimises potential for error.
Lets apply this to a few cases
Case 1
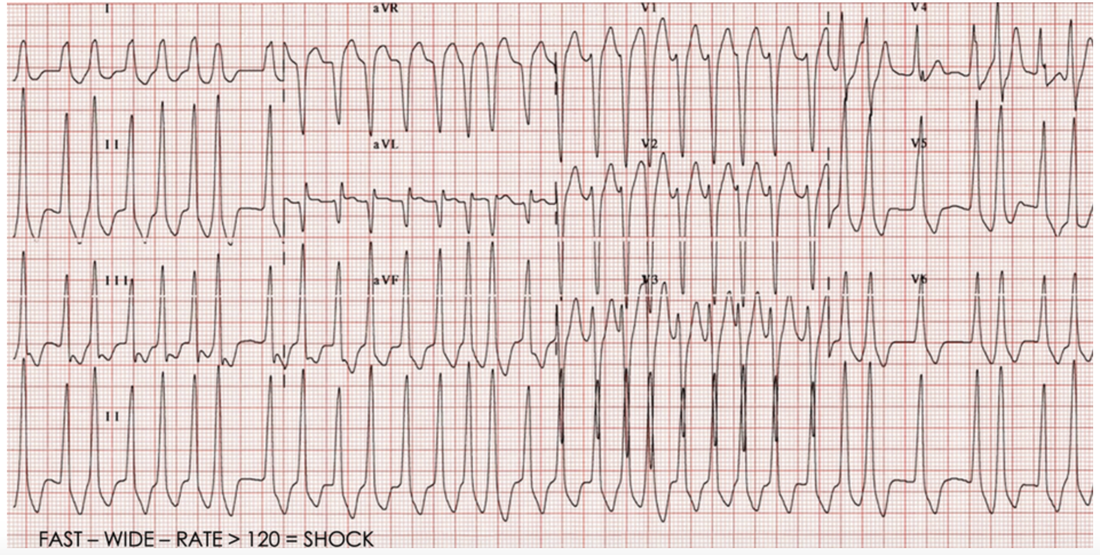
What does this ECG show and what would you do?
|
This is fast at >120 beats per minute. Its wide and narrow, because some are passing through the AV node and some are going via the accessory pathway. You can see that in some cases the rate approaches 300 beats per minute. When the rate is > 250 in an adult assume that there is an accessory pathway.. More on this in the Medications that can kill your patient section.
This is AF with WPW. An AVN blocker is contraindicated. Let's apply the treatment algorithm. In this case the rate is >120 and wide so we DC cardiovert. |
Case 2
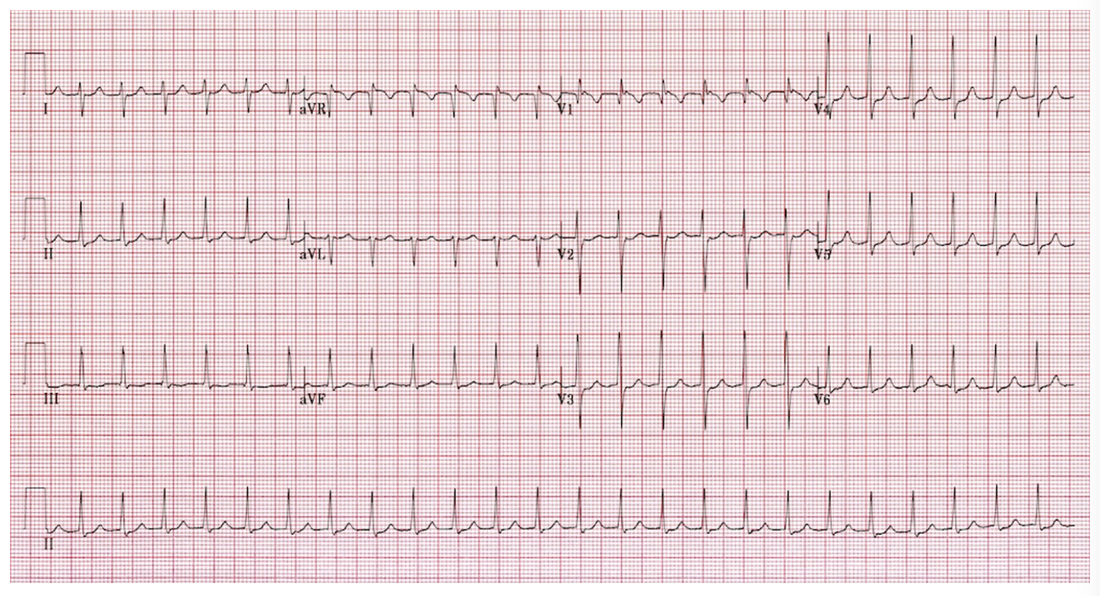
This is a 48 yo male with palpitations.
Case 3
A 45 yo male presents with palpitations. What does the ECG show? How would you treat?
|
This is a wide complex tachycardia. The diagnosis is actuallyAVNRT with LBBB. However we are not sure. The algorithm says wide complex and >120 = DC cardioversion. The safe option. What would happen if we gave an AVN blocker. Probably not much as it is regular. However I'm looking at the 2am in the morning approach(as an old boss of mine used to call it). You get the idea.
|
Watch the video on PSVT
Watch the Video on Brady-Tachy arrhythmias