Paediatric Arrhythmias and Myocarditis
Just the thought of paediatric Arrhythmias is a little scary, however you will find that they are straightforward to diagnose..
To do this, think about children as having either normal or abnormal hearts.
Those children with abnormal hearts may have potentially sinister ventricular arrhythmias and other rhythm disturbances, that you will get assistance with.
Those children with normal hearts, will mostly present with SVT. They may present with ventricular arrhythmias, however for the most part they will be benign.
Let's look at how kids present and what we must be aware of.
Very young children usually have:
Older children will present with:
To do this, think about children as having either normal or abnormal hearts.
Those children with abnormal hearts may have potentially sinister ventricular arrhythmias and other rhythm disturbances, that you will get assistance with.
Those children with normal hearts, will mostly present with SVT. They may present with ventricular arrhythmias, however for the most part they will be benign.
Let's look at how kids present and what we must be aware of.
Very young children usually have:
- Failure to Thrive
- Diaphoresis on feeding
- SOB on Feeding
- They can turn a little blue- especially those with Tetralogy of Fallot
Older children will present with:
- Lethargy
- Palpitations
- Syncope/pre-syncope
FAST AND NARROW RHYTHMS
CASE 1: 7 Month old with bronchiolitis?
A 7 month old is brought into the emergency department by his parents. He has been irritable for the past two days. Four days ago he had a fever and was taken to the family doctor who prescribed antibiotics for an ear infection. Today the mother has noticed an intermittent wheeze.
The resident sees the patient, who is afebrile and has sats of 100%. She believes the pulse is about 150, but couldn't measure it accurately as it was quite fast.
The case is presented as a case of bronchiolitis.
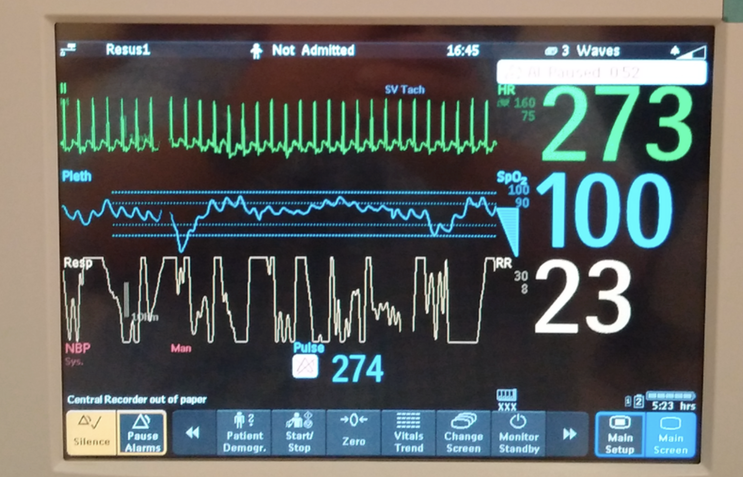
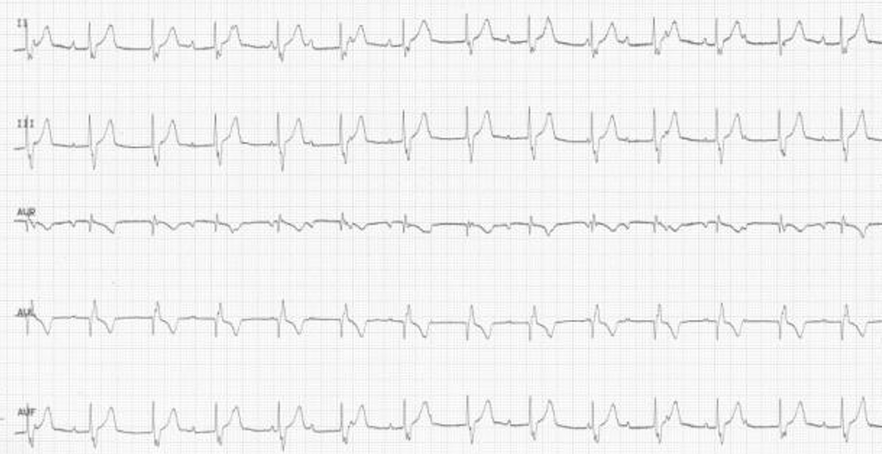
Given that we cannot get an accurate pulse reading, the baby is attached to a cardiac monitor and the result is shown below.
A 7 month old is brought into the emergency department by his parents. He has been irritable for the past two days. Four days ago he had a fever and was taken to the family doctor who prescribed antibiotics for an ear infection. Today the mother has noticed an intermittent wheeze.
The resident sees the patient, who is afebrile and has sats of 100%. She believes the pulse is about 150, but couldn't measure it accurately as it was quite fast.
The case is presented as a case of bronchiolitis.
Given that we cannot get an accurate pulse reading, the baby is attached to a cardiac monitor and the result is shown below.
|
The diagnosis is SVT.
What had most probably occurred, was that the child has had a viral illness and has gone into SVT, which has persisted for several days. The wheeze now being heard was actually cardiac failure. Children with SVT that isn't reversed can develop, cardiomegaly and cardiac failure. A simple vagal technique (ice in a bag over the face), reverted the child back into normal sinus rhythm. Are we done? Can the child go home similarly to adults? NO |
We must beware of missing the diagnosis of MYOCARDITIS in children.
A few facts on Myocarditis (1-3):
A few facts on Myocarditis (1-3):
- It has an Insidious onset
- It is usually preceded by viral illness.
- 50% cases misdiagnosed as asthma or pneumonia
- High Mortality
- 75% in Infants / 25% in young children
- Can be similar to other conditions
- Can present as heart failure or cardiogenic shock
- Causes Dilated Cardiomyopathy
Myocarditis Syndromes
- Sudden death
- In paeds is commonly associated with myocarditis
- Arrhythmias
- Palpitations can occur without cardiac failure
- Consider in all children with complete heart block
- Need implantable pacemaker.
- Ventricular arrhythmias
- Chest Pain/MI
- It may mimic MI- Troponins up in all cases(2)
- Acute heart Failure
- Classic Presentation
- Acute heart failure + Dilated Cardiomyopathy a few weeks after a viral illness- resp or gastro
- Myocarditis => 35% of dilated cardiomyopathy in children in Australia(3)
- Classic Presentation
CASE 2: A 3yo with palpitations
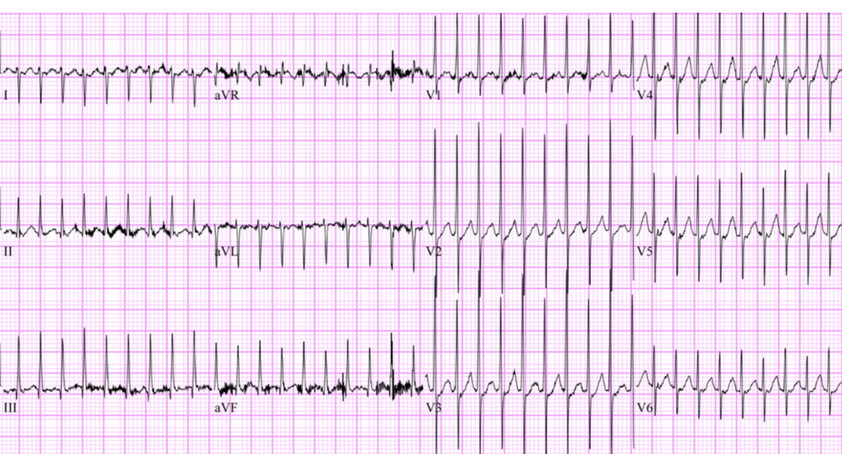
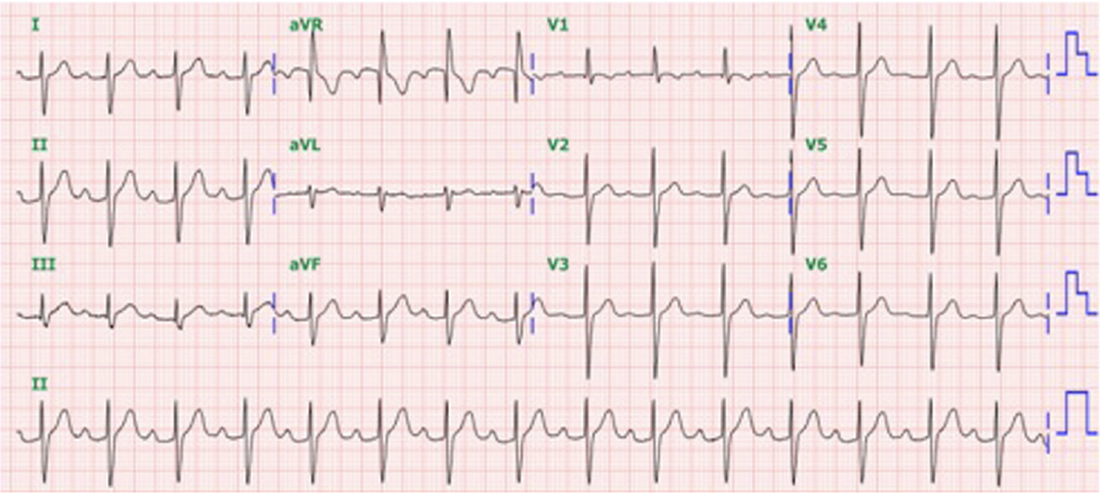
A 3yo boy is brought into the emergency department by his parents as he says that his heart 'is hitting' his chest and he felt dizzy, prior to arrival. There is no other history and the examination is normal. His ECG is shown below.
A 3yo boy is brought into the emergency department by his parents as he says that his heart 'is hitting' his chest and he felt dizzy, prior to arrival. There is no other history and the examination is normal. His ECG is shown below.
|
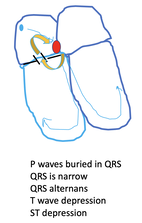
This is an SVT. The most common arrhythmia in children. It is an Atrioventricular re-entry tachycardia (AVRT), which is the most common form of SVT in children less than 10 yo.. It occurs via an accessory pathway and the rates are usually >240 bpm. There is no pre-excitation as the pathway is part of the re-entry circuit, so pre-excitation is concealed. He reverts with a vagal manoeuvre. On history it is revealed that he has also had a recent febrile illness. |
SUMMARY POINTS ON NARROW COMPLEX TACHYCARDIAS
In children Narrow Complex Tachycardias are:
- Sinus Tachycardias
- Atrial Tachycardias
- Supraventricular Tachycardias
- Most common are AVRT in the < 10yo group
- Can also have AVNRT
- A fib/flutter
- These are intra-atrial and more likely in the very young and those with a cardiac surgery history
SLOW RHYTHMS
CASE 3: A 2yo girl with lethargy, SOB and diaphoresis.
There is no other past medical history except for a recent viral illness.
Vitals are: T 37.1, HR 88 RR 16 Sats 98% on room air.
The ecg is shown below.
There is no other past medical history except for a recent viral illness.
Vitals are: T 37.1, HR 88 RR 16 Sats 98% on room air.
The ecg is shown below.
This is a complete heart block.
Complete heart blocks occur in children that may have:
Complete heart blocks occur in children that may have:
- Congenital heart disease
- Myocarditis (this patient had a febrile illness recently)
- Structural heart disease.
SUMMARY POINTS ON NARROW COMPLEX BRADYCARDIAS
The most common cause is sinus bradycardia, due to increased vagal tone or medications(beware the overdose)
Other causes include:
Other causes include:
- Sinoatrial node disease causing pauses or sick sinus syndrome
- AVN Blocks ie., 1st, 2nd and 3rd degree.
WIDE COMPLEX TACHYCARDIA
Wide Complex Tachycardias(WCT) are rare in children. Children with a cardiac history including congenital heart disease, cardiomyopathy, channelopathies or QT abnormalities, have more sinister causes of WCT. Those with no heart disease, tend to have more benign causes of WCT.
CASE 4: A 26 month old with fever.
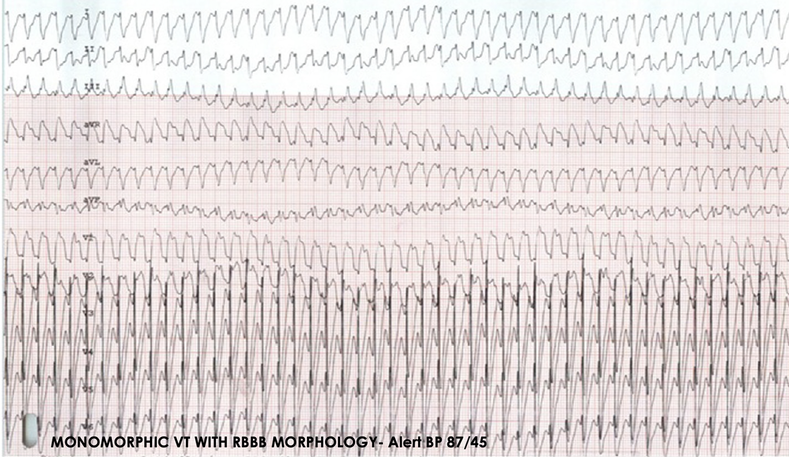
The child presents with fever and is admitted to hospital. The original ECG is shown below (4).
The child presents with fever and is admitted to hospital. The original ECG is shown below (4).
There is not much to see here. This is normal.
The temperature then rises and the following occurs.
The temperature then rises and the following occurs.
This is a wide complex tachycardia with a RBBB morphology.
It was diagnosed as VT. Initially adenosine didn’t work. Amiodarone and lignocaine were also used unsuccessfully. The patient was cardioverted. The next day the patient went back into this rhythm again and cardioversion did not work, but the arrhythmia responded to lignocaine.
No cause was found initially, but when the family was investigated, the grandfather had a Brugada pattern. This was Brugada being unmasked by fever. Go to the Brugada section for more.
It was diagnosed as VT. Initially adenosine didn’t work. Amiodarone and lignocaine were also used unsuccessfully. The patient was cardioverted. The next day the patient went back into this rhythm again and cardioversion did not work, but the arrhythmia responded to lignocaine.
No cause was found initially, but when the family was investigated, the grandfather had a Brugada pattern. This was Brugada being unmasked by fever. Go to the Brugada section for more.
Monomorphic Ventricular Tachycardia
CASE 5: A 9yo with palpitations and dizziness.
The ecg is shown below.
The ecg is shown below.
This is a Right Ventricular Outflow Tract (RVOT) Tachycardia. It occurs from a single focus in the right ventricular outflow tract.
The mean age of occurrence is 8 yo.
It is characterised by:
This condition is associated with a benign prognosis and patients are usually well with this and don't suffer syncope. Many will have a spontaneous resolution of the condition as they get older. However they do require an ECHO to exclude any structural heart disease. Treatment is usually with beta or calcium channel blockers, however ablation may also be needed.
The mean age of occurrence is 8 yo.
It is characterised by:
- LBBB Morphology and
- Positive deflection of the inferior leads
This condition is associated with a benign prognosis and patients are usually well with this and don't suffer syncope. Many will have a spontaneous resolution of the condition as they get older. However they do require an ECHO to exclude any structural heart disease. Treatment is usually with beta or calcium channel blockers, however ablation may also be needed.
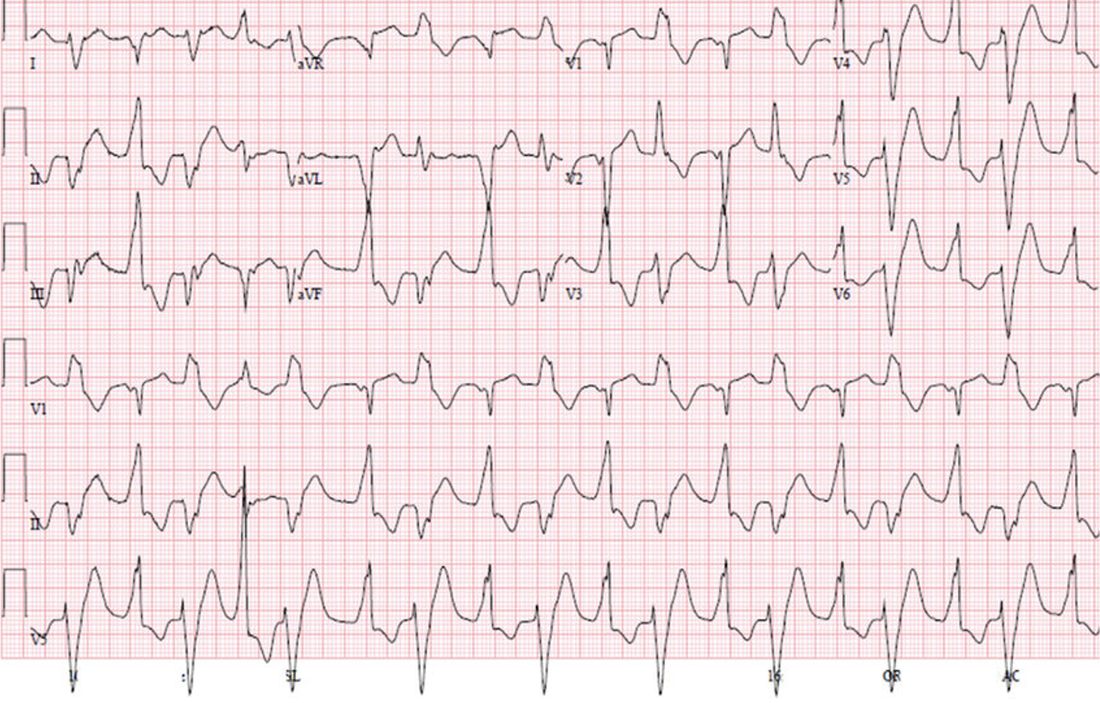
CASE 6: A 12 yo boy has palpitations during exercise
A 12 yo presents following episodes of palpitations during exercise. He has become a little dizzy on two occasions but has not lost consciousness. He has no other past medical history. His ecg is shown below.
A 12 yo presents following episodes of palpitations during exercise. He has become a little dizzy on two occasions but has not lost consciousness. He has no other past medical history. His ecg is shown below.
This is Posterior fascicular VT, which is a re-entry circuit in the left posterior fascicle.
It occurs in about 10% of cases of paediatric VT and is usually brought on by exercise and is sustained.
It is named Belhassen VT and is sensitive to verapamil.
It occurs in about 10% of cases of paediatric VT and is usually brought on by exercise and is sustained.
It is named Belhassen VT and is sensitive to verapamil.
Polymorphic Ventricular Tachycardia
This is rare in paediatric patients and is almost always associated with a cardiac abnormality. It has a worst prognosis than monomorphic ventricular tachycardia.
These patients need to be investigated for underlying disease including channelopathioes, cardiomyopathy and myocarditis, metabolic and electrolyte causes. Some may require implantable defibrillators.
These patients need to be investigated for underlying disease including channelopathioes, cardiomyopathy and myocarditis, metabolic and electrolyte causes. Some may require implantable defibrillators.
CASE 7: A 12 yo boy with syncope
A 12 yo boy presents with an episode of syncope during exertion exercise. His ecg is shown below.
A 12 yo boy presents with an episode of syncope during exertion exercise. His ecg is shown below.
This is bidirectional ventricular tachycardia, similar to what may occur, with digoxin toxicity.
In this case it is it is Catecholamine induced polymorphic tachycardia.
This is an inherited condition, that if untreated carries a 30% mortality.
It is a stress induced tachycardia that can lead to syncope or cardiac arrest and patients can suffer a VF arrest or sudden cardiac death.
Treatment is initially with a beta blocker such as Propranolol, Atenolol or Nadolol. If this fails to control the arrhythmia an implantable defibrillator may be needed.
In this case it is it is Catecholamine induced polymorphic tachycardia.
This is an inherited condition, that if untreated carries a 30% mortality.
It is a stress induced tachycardia that can lead to syncope or cardiac arrest and patients can suffer a VF arrest or sudden cardiac death.
Treatment is initially with a beta blocker such as Propranolol, Atenolol or Nadolol. If this fails to control the arrhythmia an implantable defibrillator may be needed.
References
- Chang Y, et al. Myocarditis presenting as gastritis in children. Pediatr EmergCare. 2006;22:439–40
- Kern J, et al Clinical myocarditis masquerading as acute coronary syndrome. J Pediatr. 2009;154:612–615.
- Daubeney PE, et al National Australian Childhood Cardiomyopathy Study. Clinical features and outcomes of childhood dilated cardiomyopathy: results from a national population-based study. Circulation. 2006;114:2671–2678.
- Kim G et al. A pediatric case of Brugada syndrome diagnosed by fever-provoked ventricular tachycardia. Korean J Pediatr 2014;57(8):374378
- Keone R et al. Syncope and the risk of sudden cardiac death: Evaluation, management, and prevention. Journal of Arrhythmia 33 (2017) 533–544