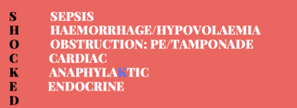
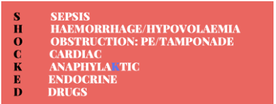
THE MNEMONIC 'SHOCKED'
|
The shocked patient can present a significant clinical challenge.
We must not fall into the trap of calling the majority of these patients, septic. Often it becomes a default because we can't think of alternatives. The SHOCKED Mnemonic can help. CASE 1 A 74 yo male presents wth a productive cough. He is febrile at 39.9 C His blood results show a raised white cell count 29 with a neutrophilia. His chest xray shows pneumonia. His BP is 65/32 Would anyone argue with a diagnosis of sepsis? THIS IS SEPSIS and starts off our mnemonic. |
CASE 2
A 75 yo male is brought into your rural emergency department with hypothermia and hypotension.
He does have a cardiac history and is on medications for hypertension.
He is commenced on the sepsis pathway and due to be retrieved to a larger centre.
He has an arterial line, which shows a pressure change when he moves.
You decide to perform a FAST exam.
It is a technically difficult exam to decipher. There is fluid there, but is it around the heart or is it in the abdomen?
A 75 yo male is brought into your rural emergency department with hypothermia and hypotension.
He does have a cardiac history and is on medications for hypertension.
He is commenced on the sepsis pathway and due to be retrieved to a larger centre.
He has an arterial line, which shows a pressure change when he moves.
You decide to perform a FAST exam.
It is a technically difficult exam to decipher. There is fluid there, but is it around the heart or is it in the abdomen?
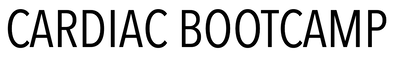
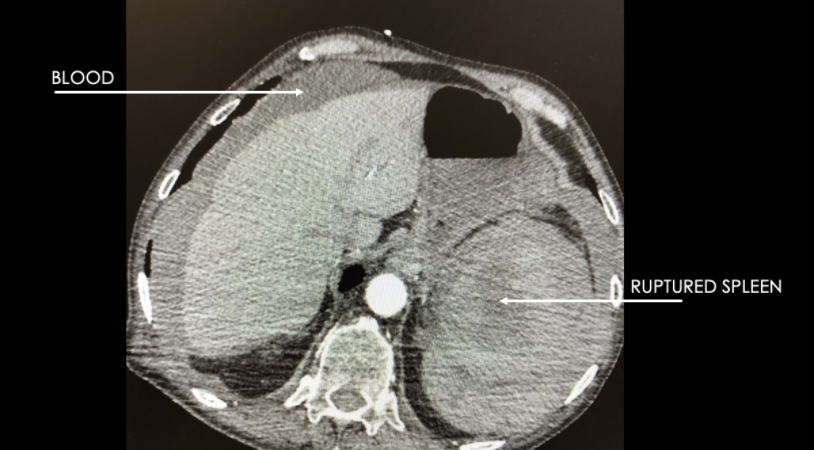
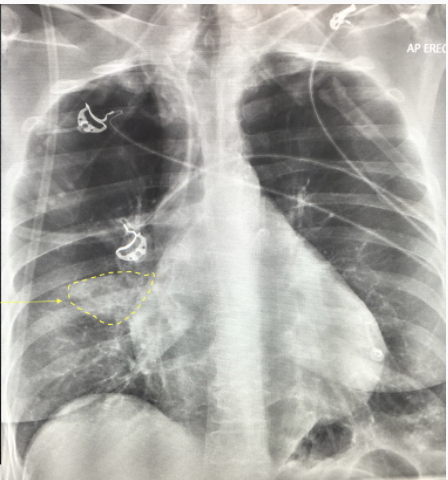
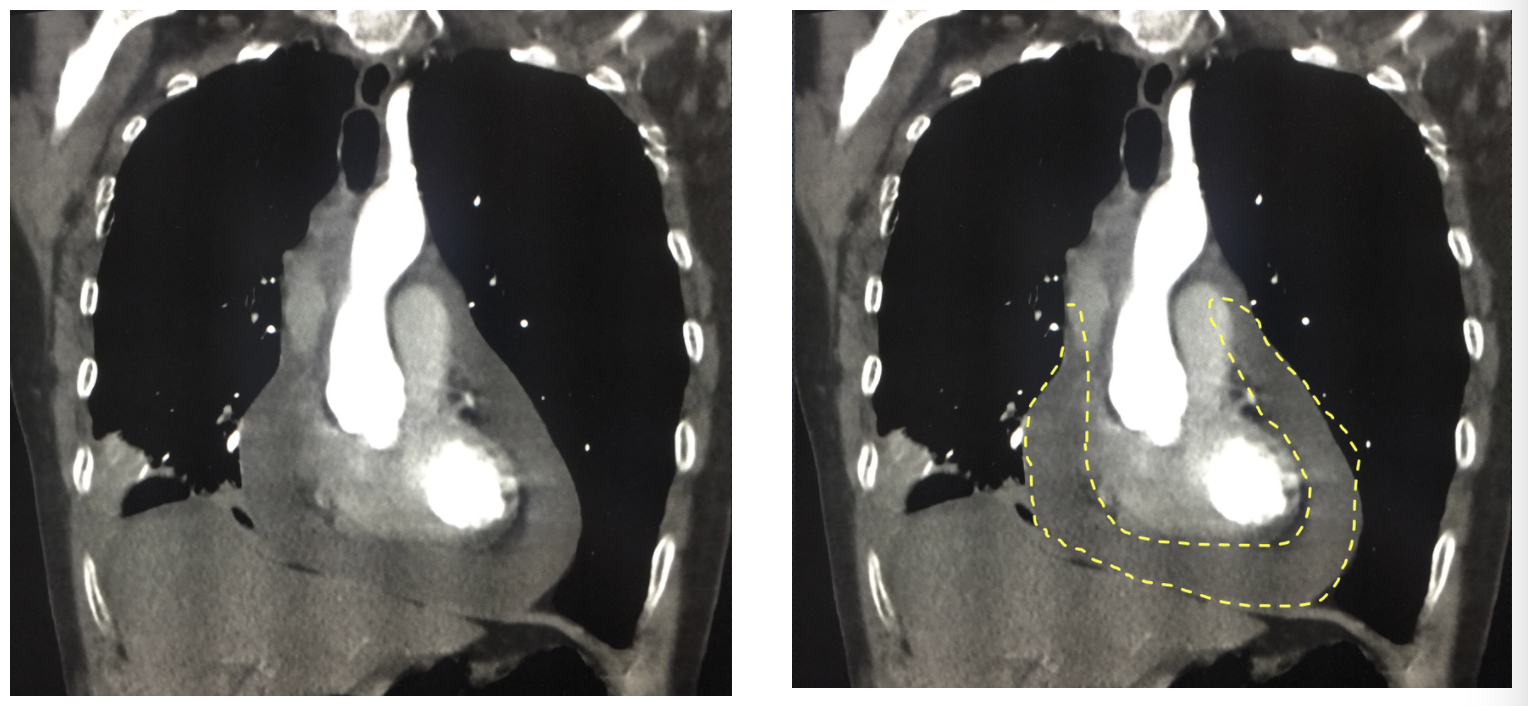
Because the Ultrasound is difficult to work out you perform a CT abdomen. One slice is shown below.
WHAT DOES THE CT ABDO SHOW?
WHAT DOES THE CT ABDO SHOW?
This gives us the second letter of our mnemonic.
Case 3
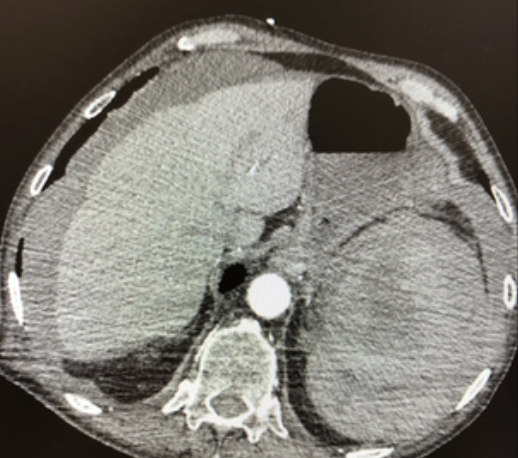
A 68 yo woman presents with shortness of breath that has been worsening over the previous 24 hours. She now has chest pain.
She is afebrile and her other vitals are:
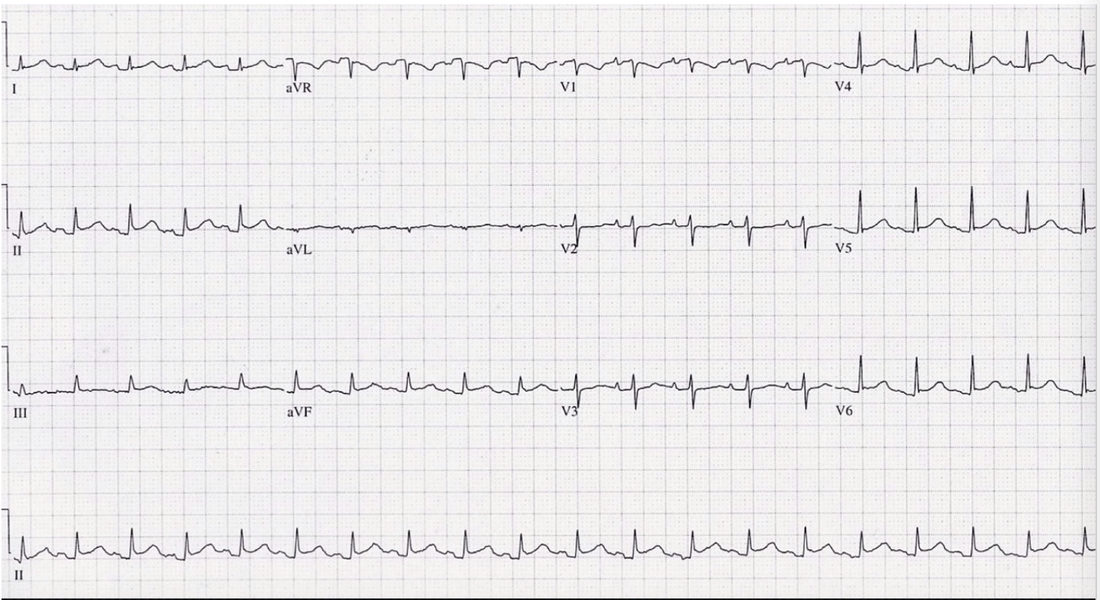
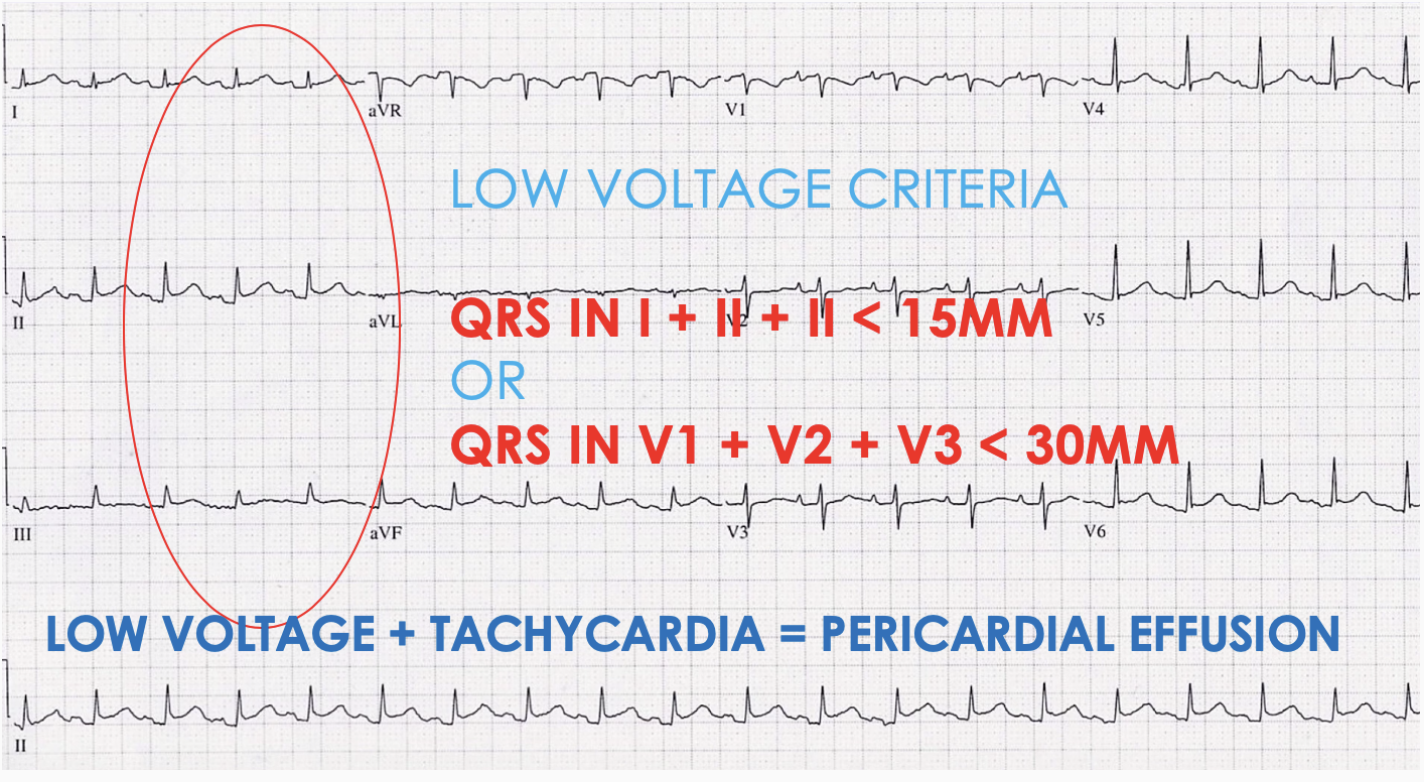
She has an ECG and a chest x-ray shown below.
The patients blood pressure continues to drop and she now has a BP of 65/32
A 68 yo woman presents with shortness of breath that has been worsening over the previous 24 hours. She now has chest pain.
She is afebrile and her other vitals are:
- Heart rate 115
- BP 87/42
- RR 31
- Sats 94% on Room air
She has an ECG and a chest x-ray shown below.
The patients blood pressure continues to drop and she now has a BP of 65/32
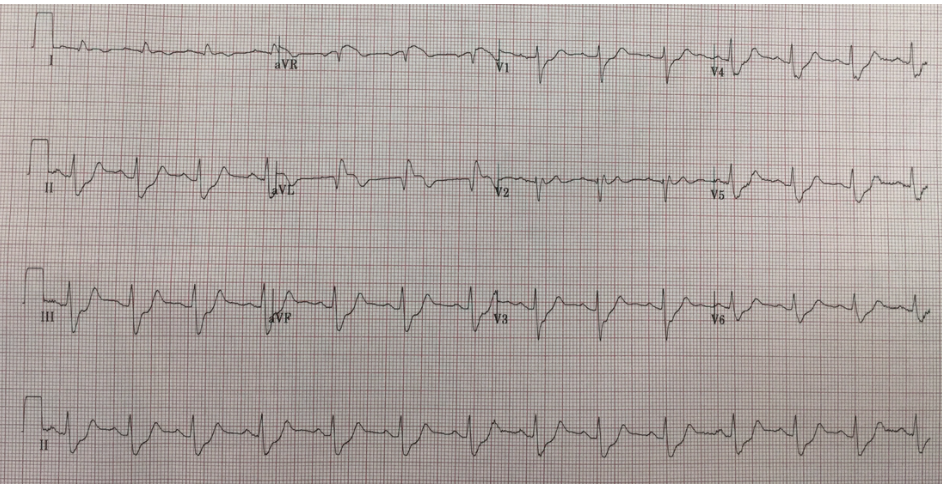
Can the ECG give us the answer? What does it show?
The patient had a CTPA and this is the result; a pericardial collection. A bedside ECHO would have helped earlier.
CASE 4
A 65 yo male is brought in by ambulance. He has chest pain and ST elevation and ST depression on his ECG.
For details go to the Cardiogenic shock module
The patient's ECG is shown below:
A 65 yo male is brought in by ambulance. He has chest pain and ST elevation and ST depression on his ECG.
For details go to the Cardiogenic shock module
The patient's ECG is shown below:
|
Case 5
A 32 yo woman presents to the emergency department with a rash and swelling to her face, following eating seafood. She is known to have an allergy to seafood, however was intoxicated and ate some at the time. She is having some trouble breathing. Her vitals are HR 112, BP 77/46. THIS IS ANAPHYLAXIS and gives us the next part of the mnemonic. Sorry, but the only way I could get it into the mnemonic was to use the 'K' in there. |
Case 6
A 33 yo woman presents to the emergency department, feeling unwell. She has had a headache and vomiting and tachycardia.
Her vitals are
On examination there are bilateral crepitations on chest auscultation and there is bilateral leg oedema.
She is placed on a sepsis pathway.........
The patient's mother arrives in the emergency department and tells you that she has a thyroid problem, but is not seeking treatment.
Beware the ENDOCRINE CAUSES
ENDOCRINE CAUSES INCLUDE:
A 33 yo woman presents to the emergency department, feeling unwell. She has had a headache and vomiting and tachycardia.
Her vitals are
- T 38
- Heart Rate 134
- BP 88/38
- Sats 98% on room air
- GCS 14
On examination there are bilateral crepitations on chest auscultation and there is bilateral leg oedema.
She is placed on a sepsis pathway.........
The patient's mother arrives in the emergency department and tells you that she has a thyroid problem, but is not seeking treatment.
Beware the ENDOCRINE CAUSES
ENDOCRINE CAUSES INCLUDE:
- Hyper/Hypothyroidism
- Adrenal Insufficiency
- Diabetic Ketoacidosis
A FEW WORDS ON THYROTOXICOSIS
We need to understand the physiology to understand the different forms of thyrotoxicosis and thus the role of antithyroid drugs
There are 2 basic causes of thyrotoxicosis
So, how do we work out the cause of this patient’s thyrotoxicosis?
Firstly, we may see clinical features of Grave’s (rapid onset, exophthalmos, diplopia, pretibial myxoedema, acropachy (soft tissue swelling of hands and clubbing of fingers)).
Next, we correlate with bloods. Patients with thyrotoxicosis typically have raised T4 and supressed TSH (though some can have isolated high T3 and normal T4, so called ‘T3 thyrotoxocosis’, and rarely the TSH will be high if there is a TSH secreting pituitary adenoma)
Then we look at antibodies. TSH-Receptor antibodies (TRAB) are almost universal in Grave’s disease, but can be present in Hashimotos. Anti-TPO antibodies and thyroglobulin antibodies can be present in Grave’s disease and Hashimotos so are poorly discriminatory.
Next, how do we treat thyrotoxic patients?
Antithyroid drugs are useful for conditions of increased TH synthesis (Graves disease, toxic adenomas and toxic multinodular goitre) but not for other causes of thyrotoxicosis. These diseases are managed by beta blockers and symptomatic treatment (see below). However, given that it often takes time to define the cause, it is reasonable to start antithyroid drugs early. Carbimazole is the drug of choice due to better compliance (once a day dosing), and the risk of fulminant hepatitis with PTU (about 1 in 10,000). Carbimazole is however teratogenic, and has a risk of agranulocytosis, so ask patients to present if they get symptoms of agranulocytosis (fever, sore throat and mouth ulcers). PTU is the drug of choice for patients who may become pregnant, and also in thyroid storm (as it decreases peripheral conversion of T4 to T3).
Antithyroid drugs take 5-10 days to have any effect, so consider starting other treatments in the interim. β-blockers are useful for palpitations, tremor and anxiety and propranolol is the drug of choice here. Benzodiazepines are occasionally needed for the anxiety/agitation.
Finally, what about thyroid storm?
This is an exaggerated form of thyrotoxicosis with a high (10-30%) mortality. Treatment needs to be started urgently on clinical grounds, without relying on confirmatory investigations. However, there are no universally accepted clinical criteria and what’s more, the T3, T4 levels are not always higher in thyroid storm when compared to uncomplicated thyrotoxicosis!
So, how do we diagnose storm? There are some clinical features to look out for
Treatment of Thyroid Storm involves
There are 2 basic causes of thyrotoxicosis
- Diseases of increased TH synthesis (Grave’s disease, Toxic adenomas and toxic multinodular goitre)
- Diseases of increased release of preformed TH (viral thyroiditis, Hasimoto’s, which can have an initial hyperthyroid phase due to inflammation releasing TH, DeQuervains’ thyroiditis etc).
So, how do we work out the cause of this patient’s thyrotoxicosis?
Firstly, we may see clinical features of Grave’s (rapid onset, exophthalmos, diplopia, pretibial myxoedema, acropachy (soft tissue swelling of hands and clubbing of fingers)).
Next, we correlate with bloods. Patients with thyrotoxicosis typically have raised T4 and supressed TSH (though some can have isolated high T3 and normal T4, so called ‘T3 thyrotoxocosis’, and rarely the TSH will be high if there is a TSH secreting pituitary adenoma)
Then we look at antibodies. TSH-Receptor antibodies (TRAB) are almost universal in Grave’s disease, but can be present in Hashimotos. Anti-TPO antibodies and thyroglobulin antibodies can be present in Grave’s disease and Hashimotos so are poorly discriminatory.
Next, how do we treat thyrotoxic patients?
Antithyroid drugs are useful for conditions of increased TH synthesis (Graves disease, toxic adenomas and toxic multinodular goitre) but not for other causes of thyrotoxicosis. These diseases are managed by beta blockers and symptomatic treatment (see below). However, given that it often takes time to define the cause, it is reasonable to start antithyroid drugs early. Carbimazole is the drug of choice due to better compliance (once a day dosing), and the risk of fulminant hepatitis with PTU (about 1 in 10,000). Carbimazole is however teratogenic, and has a risk of agranulocytosis, so ask patients to present if they get symptoms of agranulocytosis (fever, sore throat and mouth ulcers). PTU is the drug of choice for patients who may become pregnant, and also in thyroid storm (as it decreases peripheral conversion of T4 to T3).
Antithyroid drugs take 5-10 days to have any effect, so consider starting other treatments in the interim. β-blockers are useful for palpitations, tremor and anxiety and propranolol is the drug of choice here. Benzodiazepines are occasionally needed for the anxiety/agitation.
Finally, what about thyroid storm?
This is an exaggerated form of thyrotoxicosis with a high (10-30%) mortality. Treatment needs to be started urgently on clinical grounds, without relying on confirmatory investigations. However, there are no universally accepted clinical criteria and what’s more, the T3, T4 levels are not always higher in thyroid storm when compared to uncomplicated thyrotoxicosis!
So, how do we diagnose storm? There are some clinical features to look out for
- Fever is almost universal
- Tachycardia is out of proportion to the rest of the clinical signs
- Look for complicating features too
- AF, MI, heart failure, shock
- Agitation delirium coma.
Treatment of Thyroid Storm involves
- Stop new TH production
- high dose antithyroid medications, PTU preferred
- Inhibit peripheral effects of TH
- Propanolol is the β-blocker of choice, and also decreases conversion of T4 to T3
- Inhibit TH release: Lugol’s iodine (must be given >30 mins after PTU to avoid it being substrate for the storm)
- Stress dose glucocorticoids (the HPA axis is relatively depressed)
- As well as supportive care (fluids, cooling etc)
Case 7
A 78 yo male 2-3 days post tooth extraction is brought into the emergency department with a depressed level of consciousness and a temperature of 38C.
He has been diagnosed with a tooth infection and was commenced on Augmentin.
However today he was found with a GCS of 4
His vitals are:
Hi is placed on the antibiotic pathway, with antibiotics given and IV fluids commenced.
His medications bag has his antibiotics and several empty containers of diazepam. His conscious state slowly improves and he admits to taking an overdose of diazepam.
Remember that many drugs can cause hypotension.
A 78 yo male 2-3 days post tooth extraction is brought into the emergency department with a depressed level of consciousness and a temperature of 38C.
He has been diagnosed with a tooth infection and was commenced on Augmentin.
However today he was found with a GCS of 4
His vitals are:
- HR 89
- BP 79/52
- T 38
- GCS 4-6/15
Hi is placed on the antibiotic pathway, with antibiotics given and IV fluids commenced.
His medications bag has his antibiotics and several empty containers of diazepam. His conscious state slowly improves and he admits to taking an overdose of diazepam.
Remember that many drugs can cause hypotension.
There it is: A simple mnemonic to remember the causes of shock. There are many more subcategories, so make sure to read as much as you can.