The Challenge
|
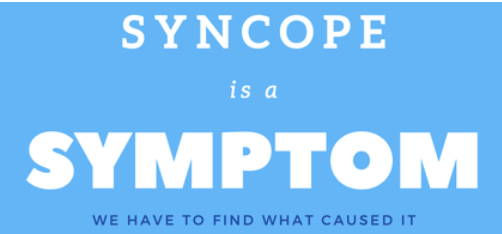
The biggest challenge we have with the patient who presents following a syncopal episode, is that syncope is a symptom of 'something'. We have to find the 'something ' that caused it. If the patient has symptoms of that 'something', it's simple. We tend to see its syncope form.... However if it's syncope alone, it can be a challenge. Syncope comprises about 5% of emergency department presentations, however I believe that that number is growing. I include Pre-syncope with syncope.
Our role again is to RISK STRATIFY our patients ie., to work out what might be benign and to pick up what may not be. That is the art. In the Syncope Rules section you can read about some of the rules. I don't believe they really help us, I believe. It comes down to good clinical medicine. |
Definition of Syncope
|
Three things must occur for an event to be called syncope.
The return to baseline is critical to this definition. Return to baseline must occur, ie the patient must have no deficit. We usually expect this to occur within 5 minutes, although it usually occurs much earlier than that. An abnormal conscious state past this first five minutes may indicate another cause such as seizure. |
For many years I've used this video as an illustration of syncope;
|
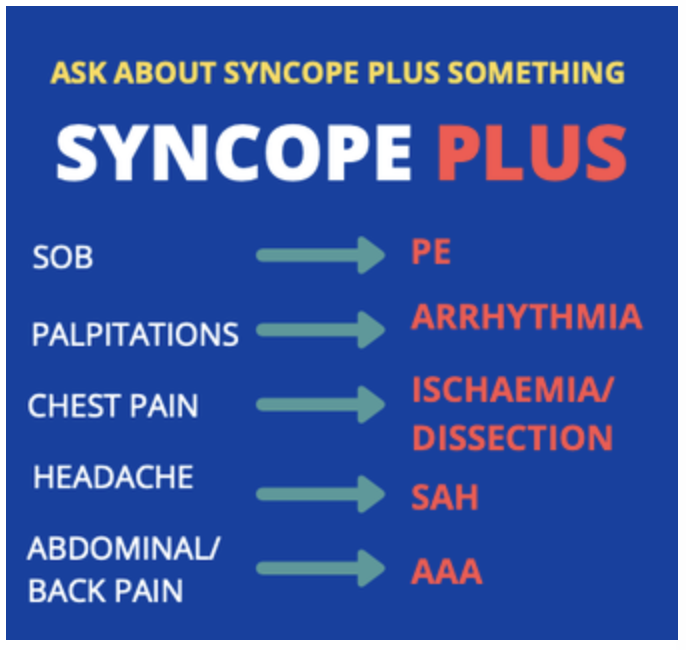
Causes of Syncope
It's Very Complex.
However the literature shows us that we can't miss the Cardiac Caused as Cardiac syncope is an independent predictor of overall mortality and cardiac mortality.
However there are other potential causes that make us nervous:
We tend to be concerned about 3 major types of causes:
Let's look at these:
However the literature shows us that we can't miss the Cardiac Caused as Cardiac syncope is an independent predictor of overall mortality and cardiac mortality.
However there are other potential causes that make us nervous:
We tend to be concerned about 3 major types of causes:
- Neurovascular
- Bleeding
- Cardiovascular
Let's look at these:
|
Neurovascular Causes
The two questions we want answered are:
In patients with TIA's secondary to vertebro-basilar insufficiency, there will usually(although not always) be symptoms of posterior circulation. In one study by Davidson (Clinical Cardiology 14,1991, 141-144,) 55% of the patients had vertigo and 46% had ataxia. Seizures can present a problem in that the collateral history can mislead us. Remember that a syncopal episode with myoclonic jerks can to a bystander look just like a seizure. Beware that the myoclonic jerks are not the result of hypoperfusion secondary to arrhythmia. What can help us determine if it is a seizure?
|
|
Bleeding Causes
What we have to think of here are the following:
These are by far the most important and include:
What we have to think of here are the following:
- Ectopic Pregnancy
- Abdominal Aortic Aneurysm
- Thoracic aortic dissection
- Gastrointestinal bleed: the action of the bleed itself can cause syncope.
These are by far the most important and include:
- Ischaemia
- Outflow Obstruction
- Cardiomyopathy
- Valve issues
- Arrhythmias
Who are the high risk patients?
The literature tells us that there are 3 groups that are at higher risk:
We need to keep the history targeted and relevant. We are looking for potential causes of the syncope, so need to know waht the patient was doing:
The literature tells us that there are 3 groups that are at higher risk:
- Older patients ie., >45 yo and certainly >65yo
- Those with a Cardiac History, which included:
- Ventricular arrhythmias
- Cardiac failure
- Those with an abnormal ECG (Review the ECG's of Syncope)
- What is considered abnormal? Any ECG that isn't normal.
We need to keep the history targeted and relevant. We are looking for potential causes of the syncope, so need to know waht the patient was doing:
- Before or during the event
- Were noxious stimuli involved, that may have provoked a vasovagal?
- What movement occurred?
- After the event
- Was the patient post-ictal?
- How quickly did they return to normal conscious state.
- Is there any relevant family history?
- Seizures?
- Arrhythmias?
- Especially any history of sudden cardiac death (remember Brugada)
- What medications is the patient on? Especially new medications.
- Could medication be dropping the blood pressure?
Examination
Please include the following as part of the examination:
There are 3 investigations I do as a minimum:
There is no evidence that other screening tests make a difference.
Review all the ECG's of Syncope and my ABC formula
Please include the following as part of the examination:
- VITALS: Look for fever and Blood Pressure abnormalities, hypoxia
- TONGUE BITING: If it's present consider just calling it a seizure, however lateral vs anterior tongue bitting may discriminate.
- INCONTINENCE
- CARDIAC: Murmurs(MI/AS), cardiomegaly(outflow obstruction)
- RESPIRATORY: Failure
- NEUROLOGICAL: Any deficits, including a Todd's paresis
- ABDOMINAL: Pulsatile masses, rectal examination looking for malaena.
There are 3 investigations I do as a minimum:
- Hb/HCT: Certainly helpful in anaemia. However an acute bleed may not show for up to 24 hours.
- Pregnancy Test: Ectopic
- ECG: The ECG has a < 5% yield in syncope(Ann Emerg Med 1984)
There is no evidence that other screening tests make a difference.
Review all the ECG's of Syncope and my ABC formula