TAKOTSUBO CARDIOMYOPATHY
A 43 yo female presents with chest pain. It had occurred following a family tragedy. Her chest pain began whilst she was in ICU visiting her family member. (This case is taken from the literature)(1)
On arrival to the emergency department, her pain was 10/10. She was diaphoretic and vomiting.
Her vital signs in the emergency department were:
HR 109 bpm
BP 101/78 mmHg
RR 2o breaths/min
O2sat 97% on RA
Examination was normal.
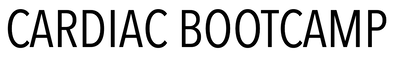
Her ECG is shown below:
On arrival to the emergency department, her pain was 10/10. She was diaphoretic and vomiting.
Her vital signs in the emergency department were:
HR 109 bpm
BP 101/78 mmHg
RR 2o breaths/min
O2sat 97% on RA
Examination was normal.
Her ECG is shown below:
, ST Elevation in in I and aVL and V1-V3
Cardiac markers were raised.
Cardiac catheterisation showed:
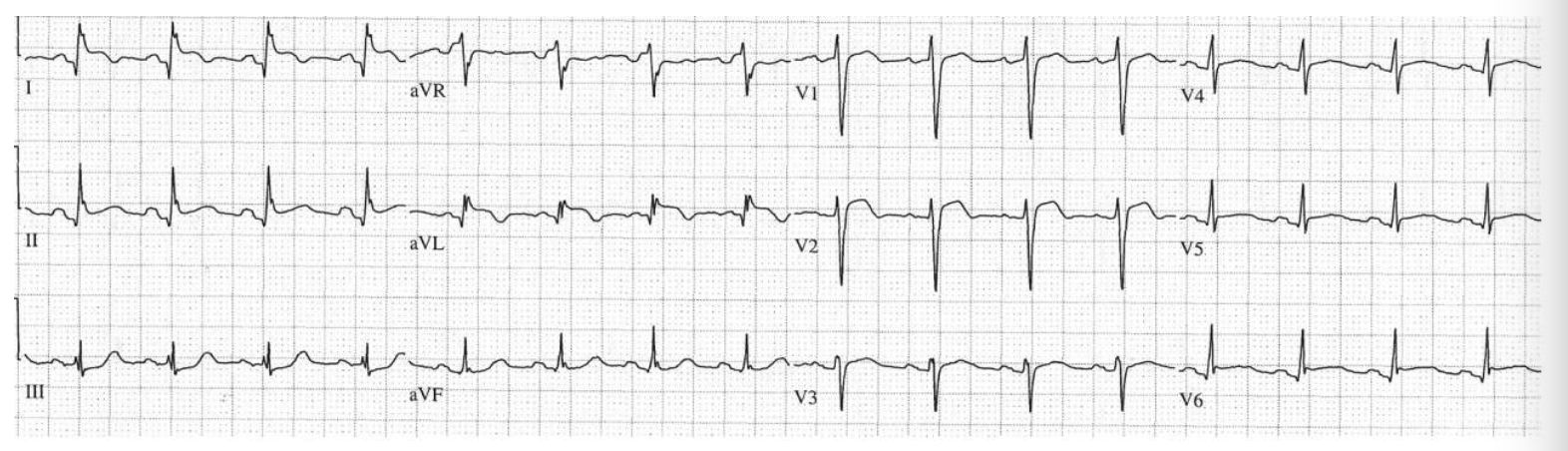
Below is her ECG at day 1. Notice the large T wave inversion in I, II, aVL and V2-V6. There is a prolonged QT.
, ST Elevation in in I and aVL and V1-V3
Cardiac markers were raised.
Cardiac catheterisation showed:
- Normal coronary arteries
- Severe hypokinesis of LV anteroapical wall, with apical ballooning.
Below is her ECG at day 1. Notice the large T wave inversion in I, II, aVL and V2-V6. There is a prolonged QT.
Case 2
Here is another case
A 64 yo woman is brought to the ED with chest pain. She had been visiting her sick husband on the ward.
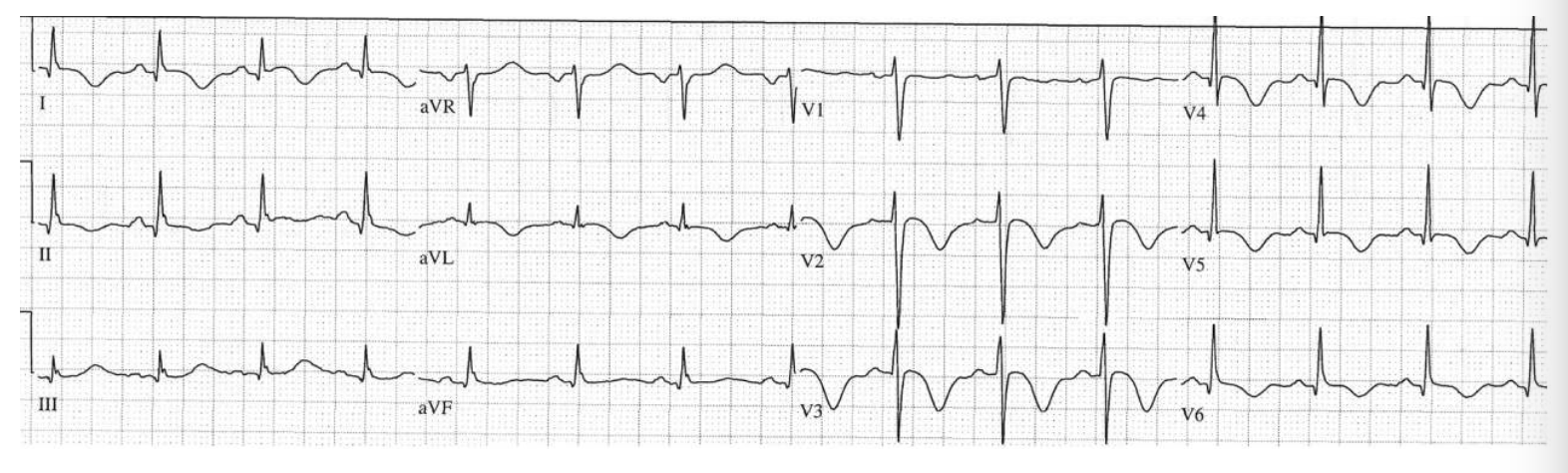
Her ECG is shown below.
It looks like a STEMI, but again it's Takotsubo.
A 64 yo woman is brought to the ED with chest pain. She had been visiting her sick husband on the ward.
Her ECG is shown below.
It looks like a STEMI, but again it's Takotsubo.
Answer
NOW LET's GO DEEP
Below is a summary based on the International Expert Consensus Document on Takotsubo Syndrome(1,2)
Epidemiology
Takotsubo Syndrome accounts for up to 3% of all patients presenting with potential STEMI. The incidence is higher in female patients. About 90% of patients are women with a mean age of 67-70 years. However, this is not a disease that only affects adults. It is also described in children.
It can recur in 5% of cases and does so within 3 weeks and 3.8 years.
It was first described in Japan in 1990 and was initially thought to be a disorder that affected only patients of Asian descent. However, we now see it in all parts of the world and in all races.
It’s been called ‘broken heart syndrome’, ‘stress cardiomyopathy’ and ‘apical ballooning syndrome’. The initial name of Takotsubo was a Japanese word for an octopus trap and described the shape of the left ventricle at the end of systole. It is called a syndrome as there are a range of triggers, both emotional and physical that lead to a condition that appears similar to acute coronary syndrome and results in the left ventricular dysfunction.
It can recur in 5% of cases and does so within 3 weeks and 3.8 years.
It was first described in Japan in 1990 and was initially thought to be a disorder that affected only patients of Asian descent. However, we now see it in all parts of the world and in all races.
It’s been called ‘broken heart syndrome’, ‘stress cardiomyopathy’ and ‘apical ballooning syndrome’. The initial name of Takotsubo was a Japanese word for an octopus trap and described the shape of the left ventricle at the end of systole. It is called a syndrome as there are a range of triggers, both emotional and physical that lead to a condition that appears similar to acute coronary syndrome and results in the left ventricular dysfunction.
Diagnostic Criteria
Patients present very similarly to those have an acute myocardial infarction (AMI). They can have chest pain, palpitations, dyspnoea and syncope. They can also present with symptoms related to its complications ie., heart failure, stroke, cardiogenic shock and cardiac arrest.
Diagnosing Takotsubo can be challenging, given that it presents similarly to AMI, both in terms of ECG changes and elevation of cardiac markers. The only way to reliably diagnose it is to perform coronary angiography and left ventriculography.
A complicating factor is that coronary occlusive lesions can occur concurrently.
There is no worldwide consensus on Diagnostic Criteria. There are multiple criteria available including:
The InterTAK diagnostic criteria, are as follows:
Diagnosing Takotsubo can be challenging, given that it presents similarly to AMI, both in terms of ECG changes and elevation of cardiac markers. The only way to reliably diagnose it is to perform coronary angiography and left ventriculography.
A complicating factor is that coronary occlusive lesions can occur concurrently.
There is no worldwide consensus on Diagnostic Criteria. There are multiple criteria available including:
- The Mayo Clinic Diagnostic Criteria
- The Japanese Guidelines
- The Gothenburg Criteria
- The Johns Hopkins Criteria
- The Tako-tsubo Italian Network Proposal
- Criteria of Heart Failure Association Taskforce of European Society of Cardiology
The InterTAK diagnostic criteria, are as follows:
- Postmenopausal women are more commonly affected
- Emotional + physical triggers can precede it, but is not obligatory
- Significant coronary artery disease is not a contraindication to the syndrome
- Concommitant CAD can be present and ranges from 10-29%
- Neurological disorders (SAH, stroke/TIA or seizures) may be a trigger
- Pheochromocytoma may be a trigger
- New ECG abnormalities are present as below, however rarely there may be no ECG changes:
- ST segment elevation
- T wave inversion
- QTc prolongation
- Cardiac biomarkers are moderately raised
|
Pathophysiology
Sympathetic Stimulation appears to be the cause of this condition. Triggering by emotional or physical triggers is the main cause, however it is also associated with catecholamine access such as occurs in pheochromocytoma and central nervous system disorders. The release of catecholamines in some patients with increased susceptibility of coronary microcirculation and cardiac myocytes, can lead to LV dysfunction and secondary myocardial inflammation. Hypotheses for how this occurs include:
What are the Triggers? Triggers can be both emotional or physical, or a combination of the two. Males are more often affected by physical stressors and women by emotional stressors. Emotional triggers don’t have to be negative. Positive emotional triggers can also produce the syndrome, giving rise to the description ‘Happy Heart Syndrome’. Physical stressors can be related to physical activities such as sports, to medical conditions, procedures or traumatic injury. |
What Predisposes patients to Takotsubo Syndrome?
Hormonal Factors Women older than 55 years of age have 5 times the risk than those less than 55 years of age. Given the significant number of post-menopausal women that are susceptible to this syndrome, it is thought that declining oestrogen levels increase susceptibility. Oestrogen can decrease the sympathetic response to stress. Genetic Factors Familial cases of Takotsubo have been reported raising the likelihood that there is a genetic predisposition. Psychiatric and Neurological Disorders Rates of psychiatric and neurological disorders was much higher in Takotsubo patients. Studies have shown that depression and anxiety is much higher in these patients. Patients with depression have an exaggerated noradrenaline response to stress and may have a decrease noradrenaline reuptake. It can also occur following a stroke or a subarachnoid haemorrhage or a seizure. The following are independent predictors of death:
|
Types of Takotsubo Syndrome
|
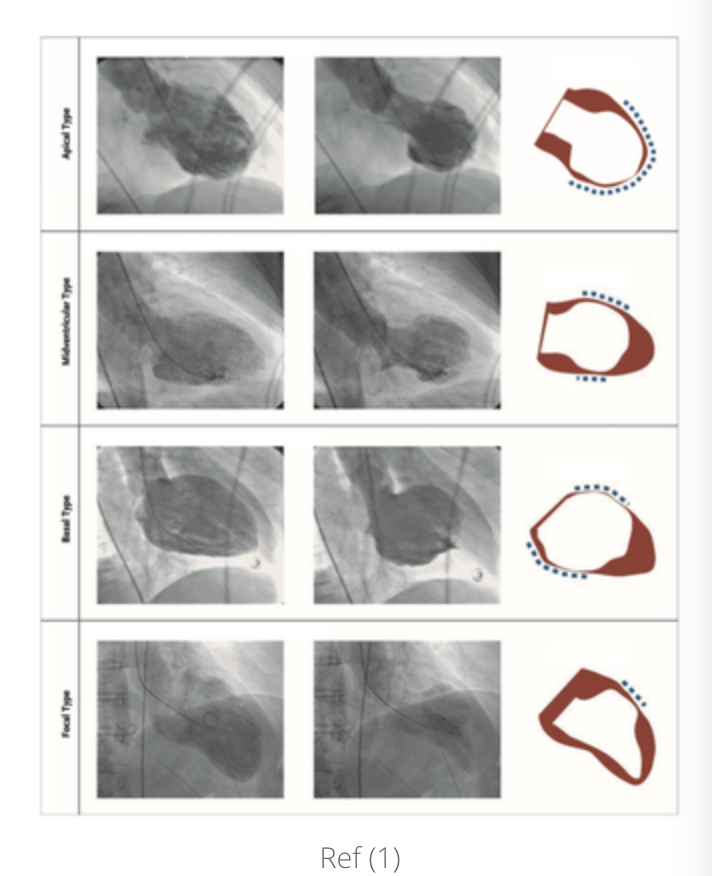
There are 4 types based on the distribution of regional wall abnormalities. These are:
|
Investigations
|
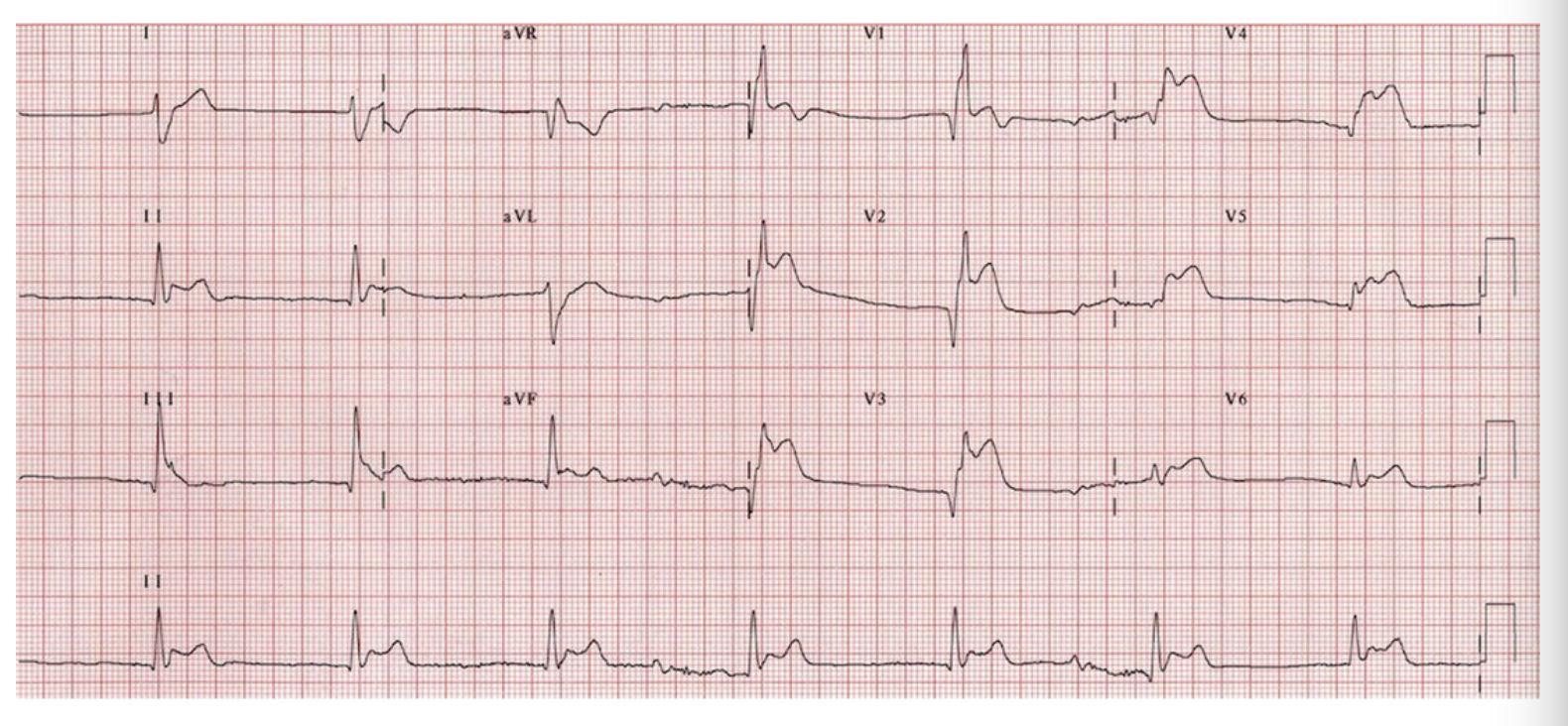
ECG
The initial ECG is abnormal in most patients. Specifically, there is ST elevation and T wave inversion, or both. There is a progression with ST elevation, followed by T wave inversion and QT interval prolongation, over several days. This is followed by resolution of over days or weeks. ST Elevation It is usually in the:
T wave inversion These are progressive changes. However, in the patient who presents late, they may be the only changes to find, given that ST elevation may no longer be present.. T wave inversion may represent myocardial stunning. It is usually more prominent than in ACS. It may persist for several months as it is associated with myocardial oedema. QT interval prolongation This may predispose patients to developing torsades de pointes and is a prognostic marker for sudden cardiac death. Anterior Q waves These represent poor R wave progression and occur frequently. Low QRS voltage This occurs frequently and is due to myocardial oedema |
Can we use ECG criteria to distinguish between Takotsubo and a STEMI? The following criteria have a high sensitivity and specificity for Takotsubo and assist in distinguishing it from anterior STEMI, however there is considerable overlap. The criteria are:
|
|
BIOMARKERS
Cardiac Markers Cardiac troponin is raised equally to that of ACS B-type natriuretic peptide and N-terminal prohormone of brain natriuretic peptide. Takotsubo is associated with a large increase in these two markers. The degree of rise of NT-proBNP is related to:
|
IMAGING
Coronary angiography and ventriculography Angiography is performed in the setting of ST elevation. If there is coexisting coronary artery disease ventriculography is used to perfusion-contraction mismatch. Echocardiography It is used to assess the changes in left ventricular function. Left ventricular contractility recovers completely in 4-8 weeks. Cardiac computed tomography angiography (CCTA) This can be performed when comorbid or other conditions do not make angiography an option. It gives information on coronary artery anatomy and regional LV contraction. Cardiac Magnetic Resonance imaging More for the subacute than the acute phase. Cardiac Nuclear Imaging SPECT can be used to test perfusion, metabolism and innervation |
Complications and Outcomes
Takotsubo is often considered a benign reversible disease. However, this is not the case and cardiogenic shock and mortality is similar to those patients with ACS
Complications in Terms of Frequency
Treatment is based on expert consensus as no prospective studies exist.
A few words about general medications that may be used:
- Acute heart failure (12-45%)
- Left Ventricular Outflow Tract Obstruction LVOTO (10-25%)
- Mitral regurgitation (14-25%)
- Cardiogenic Shock (6-20%)
- Atrial fibrillation (5-15%)
- LV Thrombus (2-8%)
- Cardiac Arrest (4-6%)
- AV Block (5%)
- Occurs due to increased vagal tone
- Tachy/Brady arrhythmias (2-5%)
- Ventricular Arrhythmias
- Torsades de Pointes (2-5%)
- These occur in the subacute phase (days 2-4). They coincide with a lengthening of the QT interval and anterolateral T wave inversion.The most malignant episodes are associated wit QTc >500ms.
- VT/VF (3%)
- Torsades de Pointes (2-5%)
- Death (1-4.5%)
- Acute ventricular septal defect (<1%)
Treatment is based on expert consensus as no prospective studies exist.
A few words about general medications that may be used:
- Catecholamine drugs in Takotsubo are associated with a 20% mortality
- Beta Blockers may improve LVOTO but are contraindicated in bradycardia and in acute severe heart failure with low LVEF and hypotension
- Angiotensin Converting Enzyme inhibitors and Angiotensin II receptor Blockers may facilitate LV recovery
- Diuretics can be used in Pulmonary oedema
- Nitroglycerin reduces afterload and left and right ventricular filling pressures in heart failure. However, they should be avoided in LVOTO as they worsen the pressure gradient
- Any drugs that prolong QTc should be used with caution as may precipitate Torsades.
Treatment of Heart Failure
|
MILD TAKOTSUBO/NO HEART FAILURE
|
HEART FAILURE/PULMONARY OEDEMA
|
CARDIOGENIC SHOCK
In LVOTO
|
Treatment of Arrhythmias
Ventricular arrhythmias (VT, VT Torsades de pointes, long QTc) AV Block
- Consider
- Beta Blocker
- Temporary RV pacing in AV Block
- Avoid
- Drugs that prolong QT interval
- Beta blocker in bradycardia and QTc > 500ms
Treatment of Thrombosis and/or Embolism
- Consider anticoagulation if LVEF < 30% or large LVD
REFERENCES
- Merchant EE et al. Takotsubo Cardiomyopathy: A Case series and Review of the Literature. West J Emerg Med. 2008 May; 9(2):104-111
- Ghadri et al. International Expert Consensus Document on Takotsubo Syndrome(part 1): Clinical Characteristics, Diagnostic Criteria and Pathophysiology. European Heart Journal(2018).39, 2032-2046
- Ghardi et al. International Expert Consensus Document on Takotsubo Syndrome (Part II): Diagnostic Workup, Outcome and Management. European Heart Journal (2018) 39, 2047-2062.
- Bybee KA et al. Clinical characteristics and thrombolysis in myocardial infarctionfame counts in women with transient left ventricular ballooning syndrome. Am J Cardiol. Aug 1 2004;94(3):343-346
- Gianni M et al. Apical Ballooning syndrome or takotsubo cardiomyopathy: a systematic review. Eur Heart J July 2006:27(13):1523-29