OMI / NOMI AND STEMI EQUIVALENTS
ST elevation myocardial infarction (STEMI) and Non-ST elevation myocardial Infarction (NSTEMI) are how we decide which patients need reperfusion therapy. Thrombolytic trials showed a decreased mortality in those patients initially treated with thrombolytics when presenting with ST elevation(STE). Since this work, STE has been associated with acute coronary occlusion. However, we know that it is much more complex than this.
Larson (1) found that 15-35% of patients going to the cath lab with STE, were false positives. We also know that 25-30% of patients diagnosed with a NSTEMI have an unrecognised total occlusion(2). This leads to a delay in angiography and a missed or established infarction leading to increased mortality.
The new terminology can assist us in not missing those patients with an occlusive lesion, but no STE. Occlusive Myocardial Infarction(OMI) criteria for ECG interpretation(covered below and sometimes called STEMI equivalents), may indicate near or total occlusion of a coronary vessel without adequate collateral circulation, resulting in an acute myocardial infarction. The alternative of Non-Occlusion Myocardial Infarction (NOMI) refers to cases where there is no occlusion or, there is an occlusion, but with sufficient collateral circulation to avoid acute infarction.
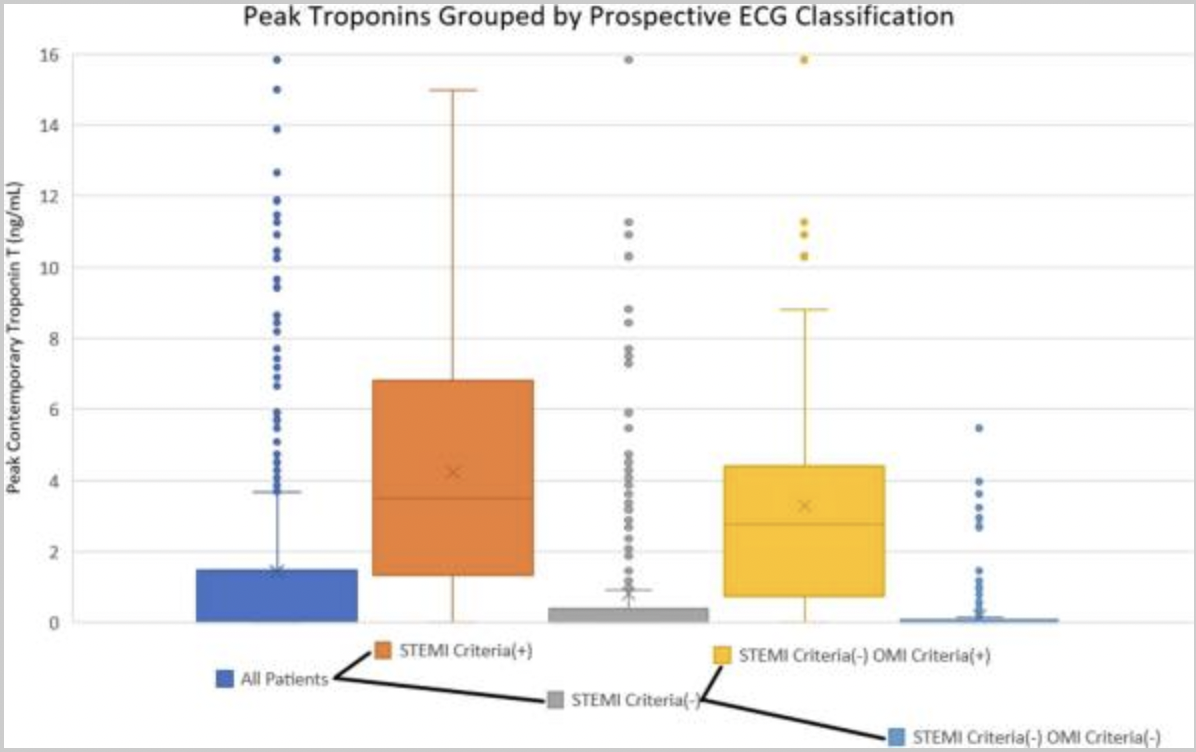
The potential benefit of using OMI instead of STEMI is clearly demonstrated by Meyers et al(3) in their retrospective study looking at the accuracy of STEMI criteria versus ECG findings that may have indicated OMI. In the graph below, patients were split into those that were STEMI +ve and STEMI -ve on ECG, then further classified as to whether they had OMI criteria.
Larson (1) found that 15-35% of patients going to the cath lab with STE, were false positives. We also know that 25-30% of patients diagnosed with a NSTEMI have an unrecognised total occlusion(2). This leads to a delay in angiography and a missed or established infarction leading to increased mortality.
The new terminology can assist us in not missing those patients with an occlusive lesion, but no STE. Occlusive Myocardial Infarction(OMI) criteria for ECG interpretation(covered below and sometimes called STEMI equivalents), may indicate near or total occlusion of a coronary vessel without adequate collateral circulation, resulting in an acute myocardial infarction. The alternative of Non-Occlusion Myocardial Infarction (NOMI) refers to cases where there is no occlusion or, there is an occlusion, but with sufficient collateral circulation to avoid acute infarction.
The potential benefit of using OMI instead of STEMI is clearly demonstrated by Meyers et al(3) in their retrospective study looking at the accuracy of STEMI criteria versus ECG findings that may have indicated OMI. In the graph below, patients were split into those that were STEMI +ve and STEMI -ve on ECG, then further classified as to whether they had OMI criteria.
|
The important part of this graph is the yellow bar, which shows patients with STEMI negative ECG criteria, but OMI positive criteria. This group of patients went on to have a large infarct.
We see that if we use STEMI criteria alone, we don’t miss acute infarctions. What we do miss is acute occlusions that may benefit from reperfusion. |
Does this really matter, as some early studies indicated that early angiography for undifferentiated NSTEMI patients does not give better outcomes(4,5)? When we look at these studies, we find that patients with persistent symptoms were not included and that the interventions, were not acute, but significantly delayed.
Definition of a STEMI
The fourth universal definition of myocardial infarction(6) gives ECG criteria that are suggestive of Acute Myocardial Ischaemia, in the absence of left ventricular hypertrophy or a bundle branch block. They are:
ST Elevation
New ST-elevation at the J-point in 2 contiguous leads with the cut-point:
ST Depression and T wave changes
New horizontal or down-sloping ST-depression ≥0.5 mm in 2 contiguous leads
and/or
T inversion >1 mm in 2 contiguous leads with prominent R wave or R/S ratio >1.
ST Elevation
New ST-elevation at the J-point in 2 contiguous leads with the cut-point:
- ≥1 mm in all leads other than
- leads V2–V3 where the following cut-points apply:
- ≥2 mm in men ≥40 years;
- ≥2.5 mm in men <40 years,
- or ≥1.5 mm in women regardless of age
ST Depression and T wave changes
New horizontal or down-sloping ST-depression ≥0.5 mm in 2 contiguous leads
and/or
T inversion >1 mm in 2 contiguous leads with prominent R wave or R/S ratio >1.
Definition of a STEMI Equivalent
These are ECG changes that represent a coronary occlusion, without showing traditional STE. These patients would benefit from percutaneous coronary intervention.(7) We can use various STEMI Equivalents to predict OMI, when STE criteria are not met. Below you will find 10 examples of STEMI equivalents.
STEMI Equivalent Examples
1. Inferior Wall Myocardial Infarction
This is diagnosed by STE in 2 contiguous inferior leads with any ST depression(STD) in aVL. AVL is the only truly reciprocal lead to the inferior wall.
STD in aVL can also help to differentiate inferior STEMI from pericarditis.
Birschof et al(8) looked at whether STD in aVL would differentiate inferior STEMI from pericarditis. They found that when there is STE in the inferior leads, any STD in aVL is highly sensitive for coronary occlusion and differentiates inferior MI from pericarditis.
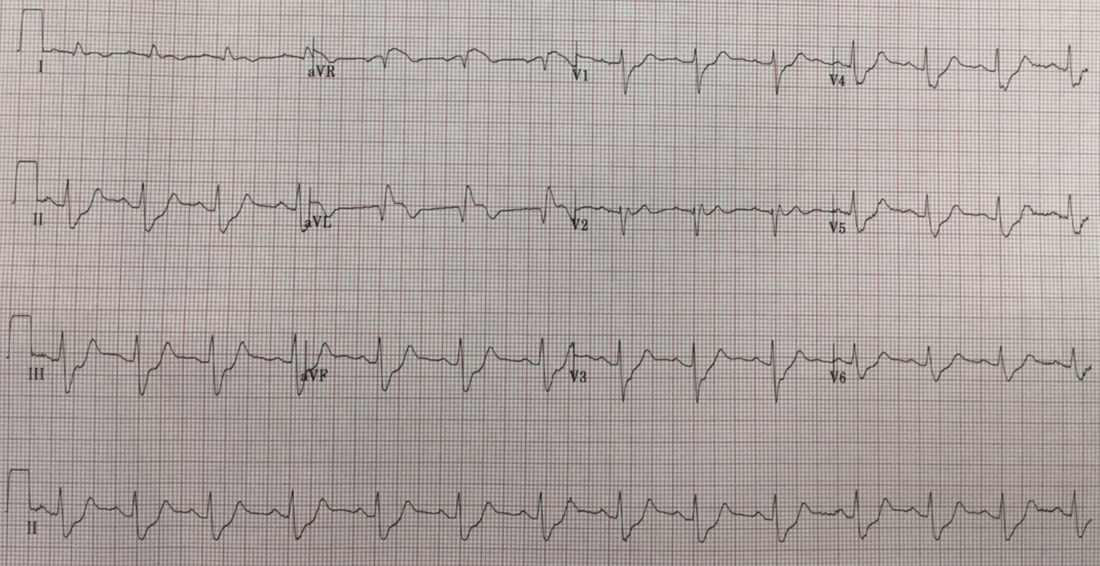
CASE
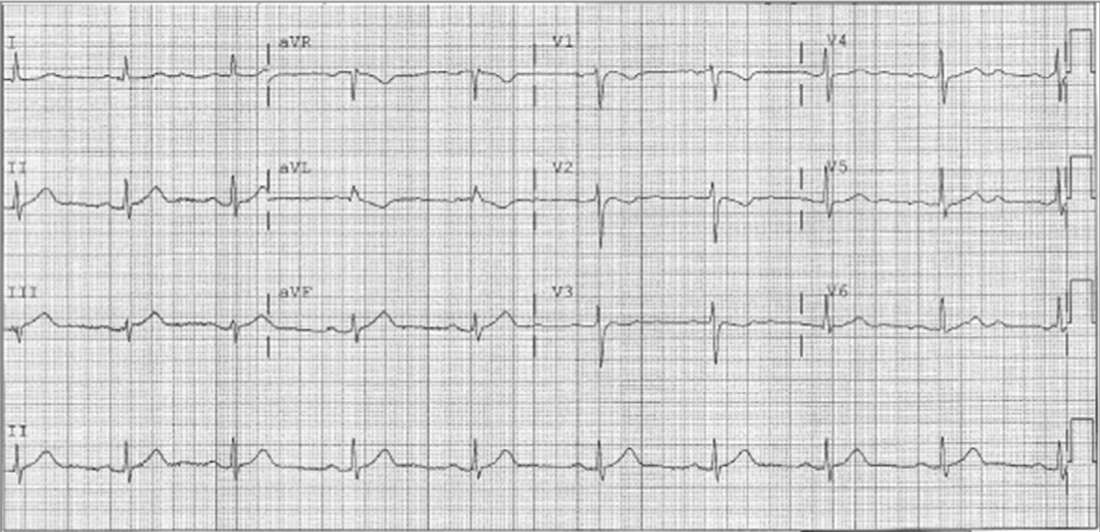
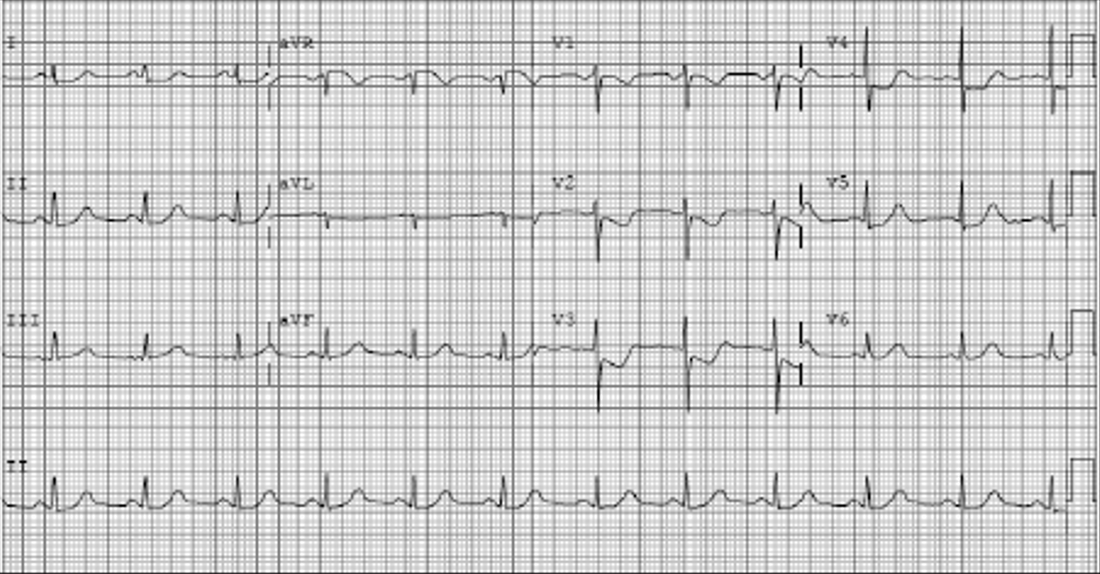
A 67 yo male presents with central chest tightness. His ECG is do and shown below.
STD in aVL can also help to differentiate inferior STEMI from pericarditis.
Birschof et al(8) looked at whether STD in aVL would differentiate inferior STEMI from pericarditis. They found that when there is STE in the inferior leads, any STD in aVL is highly sensitive for coronary occlusion and differentiates inferior MI from pericarditis.
CASE
A 67 yo male presents with central chest tightness. His ECG is do and shown below.
The ECG shows very mild STE in lead III ie., not in 2 contiguous leads. There is also a mild downsloping of the isoelectric line in II, aVF and V6, which may seem like a Spodick sign, indicating pericarditis. However there is STD in aVL. It does not fit the classical criteria for STEMI, it is a STEMI equivalent and predicts OMI. The patient had a 99% mid Right Coronary Artery occlusion.
T wave inversion in aVL is associated with impending inferior wall MI or Mid LAD lesion(10). aVL is the reciprocal lead for the inferior part of the heart.
T wave inversion in aVL is associated with impending inferior wall MI or Mid LAD lesion(10). aVL is the reciprocal lead for the inferior part of the heart.
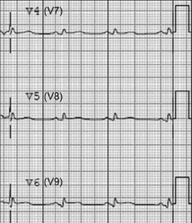
2. Posterior Myocardial Infarction
Isolated posterior MI occurs in up to 20% of AMI and is most commonly due to a left circumflex occlusion.
It is usually depicted with STD in V1-4, but no progression to V5-6. It is a recognised STEMI equivalent if there is STE in V7-9. However in some cases there is no STE in V7-9, such as in proximal circumflex occlusion.
It is usually depicted with STD in V1-4, but no progression to V5-6. It is a recognised STEMI equivalent if there is STE in V7-9. However in some cases there is no STE in V7-9, such as in proximal circumflex occlusion.
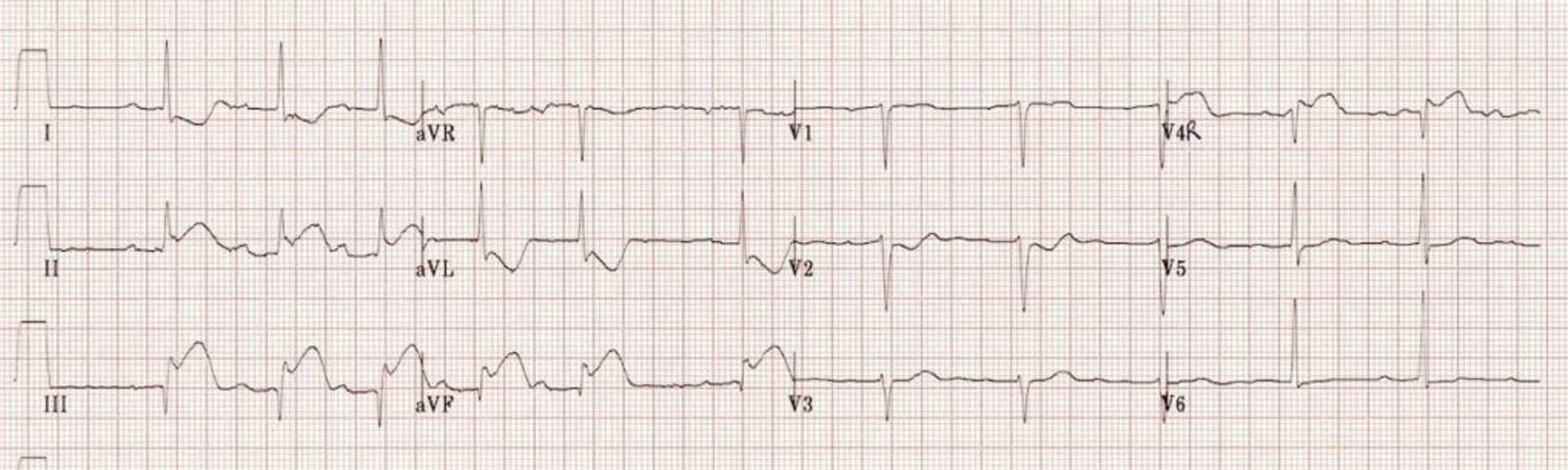
3. Right Ventricular MI
Approximately 1/3 of inferior MI’s have right ventricular involvement. In half of these patients it is of haemodynamic significance. Suspect it when see STE in V1 or inferior STE maximal in lead III. These patients require a right sided ECG leads to look for STE > 0.5mm, especially in lead V4R. STE in V4R has a high sensitivity for a high RCA occlusion.
Notice the Inferior infarction with STE III>II. V4R shows STE.
4. Hyperacute T waves
T waves are out of proportion to the preceding R waves. This especially important if there is STE and/or reciprocal changes . The T waves are wider and less symmetrical than normal T waves.
The ratio of T wave to QRS should > 0.36
Hyperacute T waves in two contiguous leads may precede STE. It is usually associated with left circumflex disease.
It presents in about 2% of proximal LAD occlusion.
The ratio of T wave to QRS should > 0.36
Hyperacute T waves in two contiguous leads may precede STE. It is usually associated with left circumflex disease.
It presents in about 2% of proximal LAD occlusion.
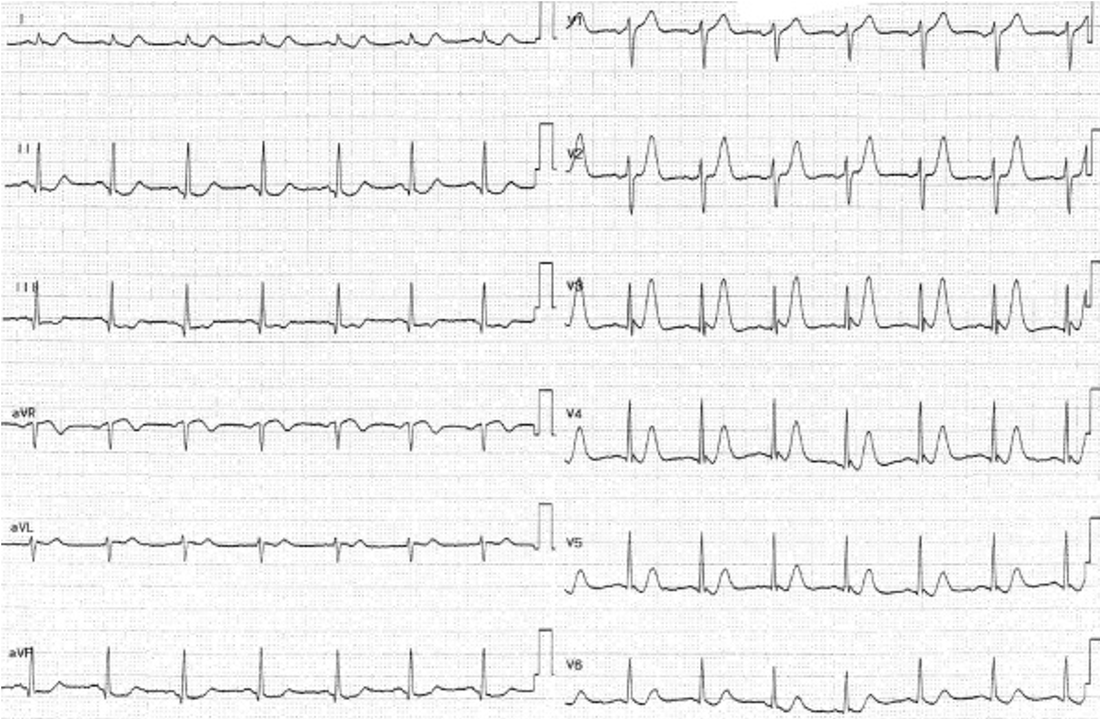
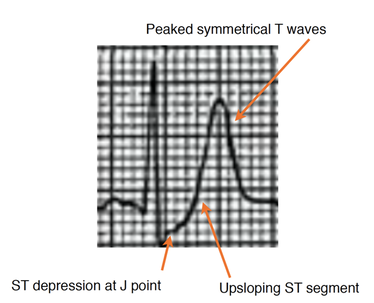
5. De Winter's T Waves
|
In De Winter's T waves there is an upsloping ST depression at the J point V1-V4 with STE. STE occurs in leads aVR + aVL. It usually indicates a proximal LAD occlusion.
The pattern was seen in the precordial leads is:
|
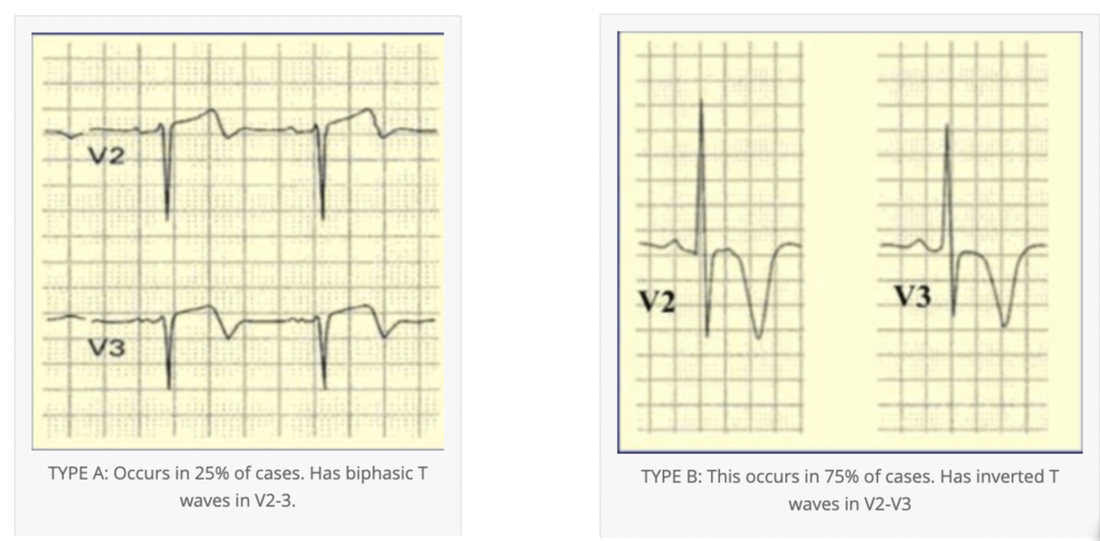
6. Wellen's Syndrome
It is a reperfusion pattern that is highly predictive of proximal LAD stenosis.
20% will have a 100% LAD occlusion with collateral flow. If not picked up 75% will progress to AMI within a week.
It presents as one of two patterns shown below.
20% will have a 100% LAD occlusion with collateral flow. If not picked up 75% will progress to AMI within a week.
It presents as one of two patterns shown below.
Wellen’s Syndrome was first described as an inverted U wave as early as 1980 and then introduced by Wellen in 1982 as Wellen’s syndrome, the name by which it is known today.
The pattern represents a significant major coronary artery stenosis. More specifically a Left Anterior Descending(LAD) artery stenosis. In most cases this is proximal, but it may be mid or distal LAD. It is a major stenosis. If the pattern is not recognised and the patient is untreated, up to 75% of patients will have an anterior wall myocardial infarction within days/weeks. Because of this it has been called “The Widow Maker”.
How to Recognise the Pattern?The peculiarity of this ECG pattern is that it may not appear when the patient has pain. In fact the only finding when the patient has chest pain, may be a small negative deflection at the end of V1 and V2 . The T waves become deeply inverted when the patient is pain free and represents a reperfusion of the myocardium. Cardiac enzymes will be normal in most cases or mildly elevated.
Characteristics of The Syndrome
The pattern represents a significant major coronary artery stenosis. More specifically a Left Anterior Descending(LAD) artery stenosis. In most cases this is proximal, but it may be mid or distal LAD. It is a major stenosis. If the pattern is not recognised and the patient is untreated, up to 75% of patients will have an anterior wall myocardial infarction within days/weeks. Because of this it has been called “The Widow Maker”.
How to Recognise the Pattern?The peculiarity of this ECG pattern is that it may not appear when the patient has pain. In fact the only finding when the patient has chest pain, may be a small negative deflection at the end of V1 and V2 . The T waves become deeply inverted when the patient is pain free and represents a reperfusion of the myocardium. Cardiac enzymes will be normal in most cases or mildly elevated.
Characteristics of The Syndrome
- Recent chest pain history
- Cardiac Enzymes normal or minimally elevated
- Deep Twaves or biphasic T wave in V2-V5 in pain free period
- No Q waves
- No Loss of R waves
- Minimal ST elevation
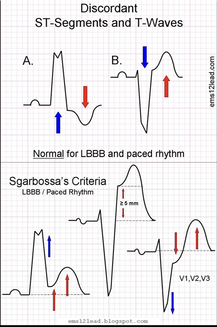
7. Left Bundle Branch Block (LBBB) and Sgarbossa.
|
A new LBBB, on it’s own, is no longer a reason to activate the cath lab. An infarction causing new LBBB would be anterior or anteroseptal, requiring a large amount of myocardial damage, which involves a large portion of the conducting system.
Diagnosing MI in LBBB can be difficult as septal activation is now the opposite of normal and there can be ST-T changes in LBBB that mask ischaemic changes. The Sgarbossa criteria with modification can assist in making the diagnosis.
A STEMI in LBBB can be diagnosed by recognising certain ECG criteria:
|
8. Right Bundle Branch Block
A new RBBB may be associated with poor outcomes in coronary artery disease (11). It indicates a proximal LAD occlusion.
Hazem(12) found a greater chance of all-cause mortality at 30 follow-up compared to those without bundle branch block. In one study(13) 26% of left main coronary occlusion presented with RBBB without STE.
When compared to patients without a RBBB. Those with a RBBB had a significantly higher 30 day mortality(14). A RBBB was found to be an independent predictor of increased mortality.
Hazem(12) found a greater chance of all-cause mortality at 30 follow-up compared to those without bundle branch block. In one study(13) 26% of left main coronary occlusion presented with RBBB without STE.
When compared to patients without a RBBB. Those with a RBBB had a significantly higher 30 day mortality(14). A RBBB was found to be an independent predictor of increased mortality.
9. Bifasicular Blocks
(RBBB + Left anterior fascicular block (LAFB)/ Left posterior fascicular block (LPFB)block)
30% of LAD occlusion presents with RBBB and LAFB(13) Refer to Fascicular Blocks blocks
30% of LAD occlusion presents with RBBB and LAFB(13) Refer to Fascicular Blocks blocks
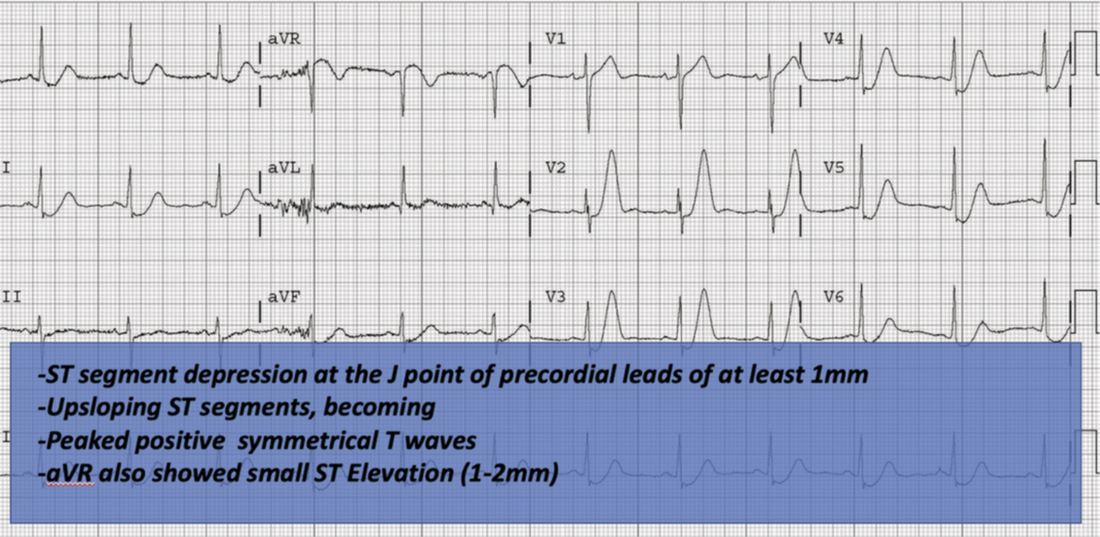
10. Diffuse ST Depression with STE in aVR
This is an example of a non-occlusive myocardial infarcdtion. It is usually due to LMCA or peoximal LAD insufficiency.
The pattern is not specific only for LMCA/proc LAD as it is also seen in pulmonary embolism, aortic dissection.
aVR looks at the right upper portion of the myocardium ie., the RV outflow tract.
If STE > 1mm in aVR or V1 with STD > 1mm in > 6 leads it can suggest:
The pattern is not specific only for LMCA/proc LAD as it is also seen in pulmonary embolism, aortic dissection.
aVR looks at the right upper portion of the myocardium ie., the RV outflow tract.
If STE > 1mm in aVR or V1 with STD > 1mm in > 6 leads it can suggest:
- Left Main coronary artery insufficiency
- Proximal LAD insufficiency
- Triple vessel disease.
References
- Larson D.M et al. ‘False-positive’ cardiac catheterisation laboratory activation among patients with suspected ST-segment elevation myocardial infarction. JAMA 298(2007) 2754-2760
- Khan A.R. et al. Impact of total occlusion of culprit artery in acute non-ST elevation myocardial infarction: a systematic review and meta-analysis. Eur Heart J. 38(2017) 3082-3089.
- Meyers H.P et al. Accuracy of OMI ECG findings versus STEMI criteria for diagnosis of acute coronary occlusion myocardial infarction. IJC Heart and Vasculature 33(2021)100767
- Mehta S.R et al. Early versus delayed invasive intervention in acute coronary syndromes. NEJM 360 (2009) 2165-2175.
- Montalescot G. et al Immediate vs delayed intervention for acute coronary syndromes: a randomised clinical trial. JAMA 302 (2009) 947-954.
- Thygesen K et al. Fourth Universal Definition of Myocardial Infarction (2018). Circulation2018;138:e618-e651
- Aslanger E.K et al. Diagnostic Accuracy oF electrocardiogram for acute coronary OCClUsion resulting in myocardial infarction (DIFOCCULT Study). IJC Heart and Vasculature. 30(2020) 100603.
- Bischof J et al. ST depression in lead aVL differentiates inferior ST-elevation myocardial infarction from pericarditis. Am J Emerg Med 2016 Feb;34(2):1490154.
- Levis J. T. ECG Diagnosis: Isolated Posterior Wall Myocardial Infarction. Perm J 2015 Fall; 19(4):e143-e144
- Birnbaum Y et al. ST segment depression in aVL: A sensitive marker for acute inferior myocardial infarction. Euro Heart J 1993;14(1):4-7
- Ahaikh S et al. New Onset Right Bundle Branch Block in Acute Coronary Syndrome and High Grade Stenosis: A Case Series. Scifed J Cardiol 2019;3(1): May.
- Hazem A et al. Is right bundle branch block associated with poor outcomes in the setting of an acute coronary syndrome? A systematic review and meta-analysis. Circ Cardiovasc Qual Outc. 7:A309
- Widimsky P et al. Primary angioplasty in acute myocardial infarction with right bundle branch block: Should new onset right bundle branch block be added to future guidelines as an indication for reperfusion therapy? Europ Heart Journal (2012) 33, 86-95.
- Kleemann T et al. MITRA PLUS Study Group: Incidence and clinical impact of right bundle branch block in patients with acute myocardial infarction: ST elevation myocardial infarction versus non ST elevation myocardial infarction. Am Heart J. 2008;156:256-261